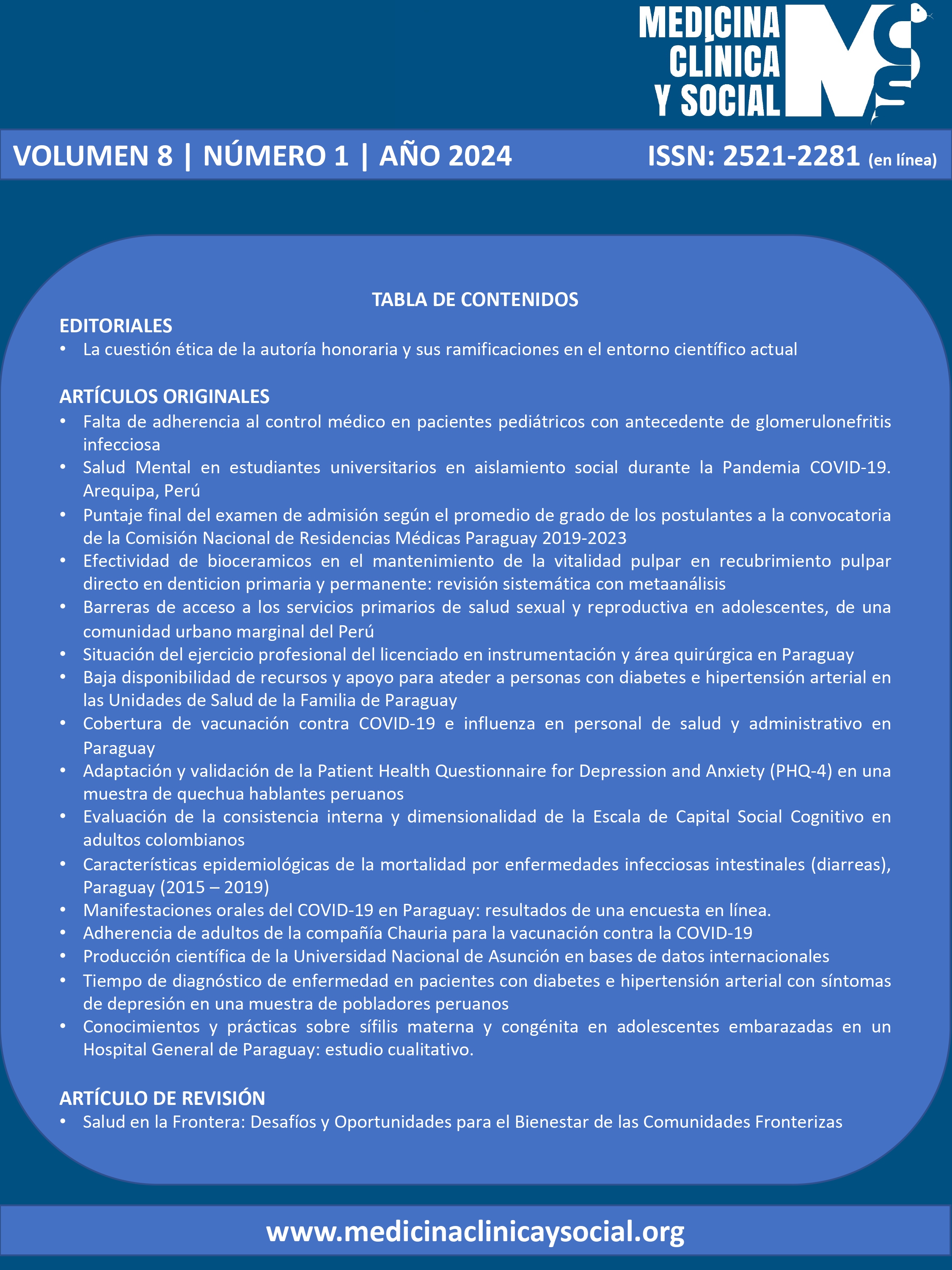
Tiempo de diagnóstico de enfermedad en pacientes con diabetes e hipertensión arterial con síntomas de depresión en una muestra de pobladores peruanos
DOI:
https://doi.org/10.52379/mcs.v8i1.302Palabras clave:
diabetes mellitus, hipertensión arterial, depresión, tiempoResumen
Introducción: La prevalencia de HTA se encuentra entre 11,9 % y 49 %, la prevalencia de DM2 es de 10,5 %. La prevalencia de trastornos depresivos en diabéticos va en el rango de 10 % a 15 %. Objetivo: determinar la asociación entre el tiempo de enfermedad de los pacientes con HTA y DM2 con los síntomas de depresión. Metodología: Estudio analítico transversal. La base secundaria analizada fue la Encuesta Demográfica y de Salud del Perú (ENDES) de los años 2019, 2020 y 2021. Se utilizó el Cuestionario de Salud del Paciente-9 (PHQ-9). Se utilizó la prueba del chi cuadrado para cada posible factor asociado a la depresión y las asociaciones de interés se evaluaron con una distribución de Poisson. Resultados: El 21,59 % tenían síntomas de depresión al momento del estudio. El 51,40 % eran del sexo femenino. El 16,58 % presentaba mayor a 60 años. La HTA estuvo presente en el 5.9%, mientras que la DM2 en el 2,09 %. En el análisis bivariado, todas las variables se asociaron con la presencia de síntomas depresivos, excepto la variable que fuma a diario (p=0.275). Discusión: Los resultados señalan una asociación entre el tiempo de enfermedad desde el diagnóstico de HTA y DM2 con los síntomas depresivos. En el caso de ambas patologías el tener menos de un año de diagnóstico aumentaban en 51 % y 44 % respectivamente la probabilidad de presentar síntomas depresivos.
Descargas
Referencias
Teck J. Diabetes-Associated Comorbidities. Primary Care. 2022;49(2): 275–286. https://doi.org/10.1016/j.pop.2021.11.004
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Research and Clinical Practice. 2022;183: 109119. https://doi.org/10.1016/j.diabres.2021.109119
Avilés-Santa ML, Monroig-Rivera A, Soto-Soto A, Lindberg NM. Current State of Diabetes Mellitus Prevalence, Awareness, Treatment, and Control in Latin America: Challenges and Innovative Solutions to Improve Health Outcomes Across the Continent. Current Diabetes Reports. 2020;20(11): 62. https://doi.org/10.1007/s11892-020-01341-9
Mendenhall E, Kohrt BA, Norris SA, Ndetei D, Prabhakaran D. Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet (London, England). 2017;389(10072): 951–963. https://doi.org/10.1016/S0140-6736(17)30402-6
Hamam MS, Kunjummen E, Hussain MS, Nasereldin M, Bennett S, Miller J. Anxiety, Depression, and Pain: Considerations in the Treatment of Patients with Uncontrolled Hypertension. Current Hypertension Reports. 2020;22(12): 106. https://doi.org/10.1007/s11906-020-01117-2
Sartorius N. Depression and diabetes. Dialogues in Clinical Neuroscience. 2018;20(1): 47–52. https://doi.org/10.31887/DCNS.2018.20.1/nsartorius
Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of Depression in Patients With Hypertension: A Systematic Review and Meta-Analysis. Medicine. 2015;94(31): e1317. https://doi.org/10.1097/MD.0000000000001317
Albasara SA, Haneef MS, Zafar M, Moinuddin KG. Depression and associated risk factors among hypertensive patients in primary health care centers in Dammam, Kingdom of Saudi Arabia. The Pan African Medical Journal. 2021;38: 278. https://doi.org/10.11604/pamj.2021.38.278.27133
Gebre BB, Deribe B, Abeto M. Magnitude and Associated Factors of Depression Among Hypertensive Patients Attending Treatment Follow Up in Chronic OPD at Hawassa University Comprehensive Specialized Hospital, Hawassa, Southern Ethiopia. Integrated Blood Pressure Control. 2020;13: 31–39. https://doi.org/10.2147/IBPC.S240015
Khan ZD, Lutale J, Moledina SM. Prevalence of Depression and Associated Factors among Diabetic Patients in an Outpatient Diabetes Clinic. Psychiatry Journal. 2019;2019: 2083196. https://doi.org/10.1155/2019/2083196
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Declaración de la iniciativa STROBE (Strengthening the Reporting of Observational Studies in Epidemiology): directrices para la comunicación de estudios observacionales. Rev Esp Salud Publica. 2008;82(3):251–9. URL.
Rantanen AT, Korkeila JJA, Löyttyniemi ES, Saxén UKM, Korhonen PE. Awareness of hypertension and depressive symptoms: a cross-sectional study in a primary care population. Scandinavian Journal of Primary Health Care. 2018;36(3): 323–328. https://doi.org/10.1080/02813432.2018.1499588
Polishchuk OY, Tashchuk VK, Barchuk NI, Amelina TM, Hrechko SI, Trefanenko IV. Anxiety and depressive disorders in patients with arterial hypertension. Wiad Lek. 2021;74(3 cz 1):455–9. URL.
Mukherjee N, Chaturvedi SK. Depressive symptoms and disorders in type 2 diabetes mellitus. Current Opinion in Psychiatry. 2019;32(5): 416–421. https://doi.org/10.1097/YCO.0000000000000528
Burns RJ, Briner E, Schmitz N. Trajectories of Depressive Symptoms and Incident Diabetes: A Prospective Study. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 2022;56(3): 311–316. https://doi.org/10.1093/abm/kaab094
Mannan M, Mamun A, Doi S, Clavarino A. Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian Journal of Psychiatry. 2016;21: 51–66. https://doi.org/10.1016/j.ajp.2015.12.008
Sensoy B, Gunes A, Ari S. Anxiety and depression levels in Covid-19 disease and their relation to hypertension. Clinical and Experimental Hypertension (New York, N.Y.: 1993). 2021;43(3): 237–241. https://doi.org/10.1080/10641963.2020.1847132
Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychotherapy and Psychosomatics. 2020;89(4): 242–250. https://doi.org/10.1159/000507639
Oliveira RA, Tostes M, Queiroz VA, Rodacki M, Zajdenverg L. Insulin mediated improvement in glycemic control in elderly with type 2 diabetes mellitus can improve depressive symptoms and does not seem to impair health-related quality of life. Diabetology & Metabolic Syndrome. 2015;7: 55. https://doi.org/10.1186/s13098-015-0052-1
Sarris J, O’Neil A, Coulson CE, Schweitzer I, Berk M. Lifestyle medicine for depression. BMC psychiatry. 2014;14: 107. https://doi.org/10.1186/1471-244X-14-107
B?descu SV, T?taru C, Kobylinska L, Georgescu EL, Zahiu DM, Z?grean AM, et al. The association between Diabetes mellitus and Depression. J Med Life. 2016;9(2): 120–125. URL.
Herder C, Hermanns N. Subclinical inflammation and depressive symptoms in patients with type 1 and type 2 diabetes. Seminars in Immunopathology. 2019;41(4): 477–489. https://doi.org/10.1007/s00281-019-00730-x
Helgeson VS, Wright A, Vaughn A, Becker D, Libman I. 14-Year Longitudinal Trajectories of Depressive Symptoms Among Youth With and Without Type 1 Diabetes. Journal of Pediatric Psychology. 2022;47(10): 1135–1144. https://doi.org/10.1093/jpepsy/jsac054
Abdoli S, Miller-Bains K, Burr EM, Smither B, Vora A, Hessler D. Burnout, distress, and depressive symptoms in adults with type 1 diabetes. Journal of Diabetes and Its Complications. 2020;34(7): 107608. https://doi.org/10.1016/j.jdiacomp.2020.107608
McInerney AM, Lindekilde N, Nouwen A, Schmitz N, Deschênes SS. Diabetes Distress, Depressive Symptoms, and Anxiety Symptoms in People With Type 2 Diabetes: A Network Analysis Approach to Understanding Comorbidity. Diabetes Care. 2022;45(8): 1715–1723. https://doi.org/10.2337/dc21-2297
Xu J, Bian Z, Zhang Y, Pan J, Gao F, Wang C, et al. Depressive symptoms in Chinese adults with risk factors for diabetes: the Shanghai High-Risk Diabetic Screen (SHiDS) study. Diabetic Medicine: A Journal of the British Diabetic Association. 2021;38(5): e14375. https://doi.org/10.1111/dme.14375
Cunanan AJ, DeWeese BH, Wagle JP, Carroll KM, Sausaman R, Hornsby WG, et al. The General Adaptation Syndrome: A Foundation for the Concept of Periodization. Sports Medicine (Auckland, N.Z.). 2018;48(4): 787–797. https://doi.org/10.1007/s40279-017-0855-3
Lu S, Wei F, Li G. The evolution of the concept of stress and the framework of the stress system. Cell Stress. 2021;5(6): 76–85. https://doi.org/10.15698/cst2021.06.250
Szabo S, Yoshida M, Filakovszky J, Juhasz G. ‘Stress’ is 80 Years Old: From Hans Selye Original Paper in 1936 to Recent Advances in GI Ulceration. Current Pharmaceutical Design. 2017;23(27): 4029–4041. https://doi.org/10.2174/1381612823666170622110046
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Joan A. Loayza-Castro, Víctor Juan Vera-Ponce

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.