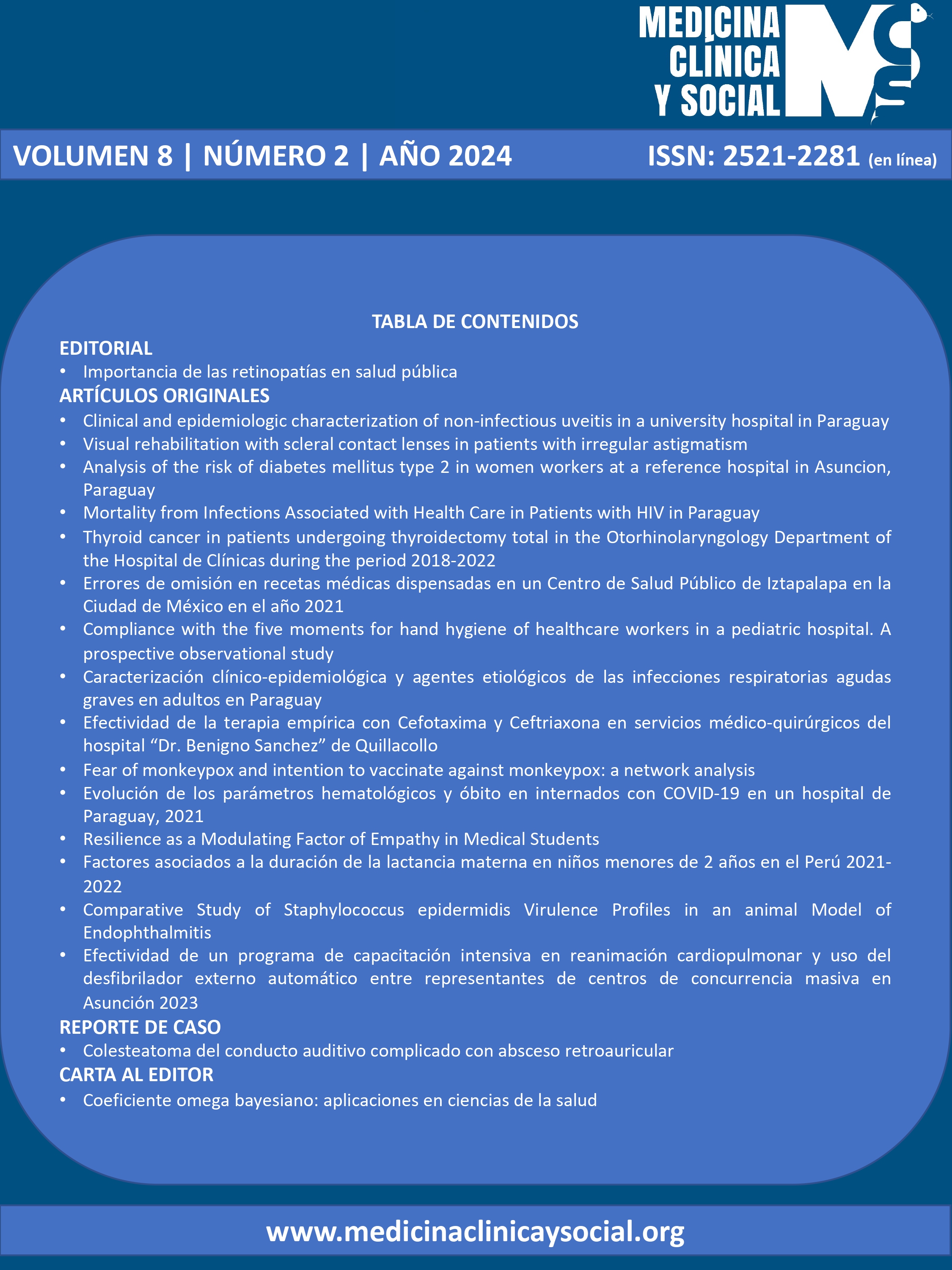
Clinical and epidemiologic characterization of non-infectious uveitis in a university hospital in Paraguay
DOI:
https://doi.org/10.52379/mcs.v8i2.346Palabras clave:
Uveitis, Non-infectiuos uveitis, clinical characterization, epidemiologyResumen
Objective: To determine the clinical and epidemiological characteristics of patients with noninfectious uveitis at a university hospital in Paraguay. Methodology: An observational, descriptive, cross-sectional, retrospective study was performed. Consecutive patients who attended the Ophthalmology Service of the Hospital de Clínicas from January 2020 to October 2021 and who were diagnosed with non-infectious uveitis were included. The variables studied were sex, age, origin, reason for consultation, anatomical classification, clinical course, systemic and ocular associations, and bilaterality. Results: A total of 78 medical records of patients meeting the inclusion and exclusion criteria were analyzed. Of the patients, 66.7% were female and 42 (53.8%) were from the Central Department. The anterior anatomical location of uveitis was the most frequent (53.9%), followed in decreasing order by panuveitis, posterior uveitis, and intermediate uveitis. Regarding anterior uveitis, 24 patients (57.1%) had unilateral uveitis, 40 (95.2%) were non-granulomatous, 19 (45.2%) presented an acute clinical course, the most frequent reason for consultation was "red and painful eye" with 15 patients (35.7%), the most frequent systemic association was HLA- B27+ in 16 patients (38.1%). As for panuveitis, 13 patients (50%) were associated with Vogt-Koyanagi-Harada syndrome, and of the latter, two patients were related to rheumatoid arthritis. Conclusion: The clinical and epidemiological patterns observed in this study were largely consistent with those reported in the literature. Notably, the most frequent associations differed from those reported in the literature: HLA-B27+ for anterior uveitis, rheumatoid arthritis for posterior uveitis, and a significant percentage of Vogt-Koyanagi-Harada syndrome among panuveitis cases.
Descargas
Referencias
Miserocchi E, Fogliato G, Modorati G, Bandello F. Review on the Worldwide Epidemiology of Uveitis. Eur J Ophthalmol. 2013;23(5):705–17. https://doi.org/10.5301/ejo.5000278
Tsirouki T, Dastiridou A, Symeonidis C, Tounakaki O, Brazitikou I, Kalogeropoulos C, et al. A Focus on the Epidemiology of Uveitis. Ocul Immunol Inflamm. 2018;26(1):2–16. https://doi.org/10.1080/09273948.2016.1196713
Calvo Hernández LM, Bautista Salinas RM, Suárez Cabrera M. Uveítis: Un reto para el internista. An Med Interna. 2008;25:141–8. http://dx.doi.org/10.4321/S0212-71992008000300009
Lightman S. Uveitis: what do we know and how does it help? Clin Experiment Ophthalmol. 2001;29(2):48–51. https://doi.org/10.1046/j.1442-9071.2001.d01-2.x
Thorne JE, Suhler E, Skup M, Tari S, Macaulay D, Chao J, et al. Prevalence of Noninfectious Uveitis in the United States: A Claims-Based Analysis. JAMA Ophthalmol. 2016;134(11):1237–45. https://doi.org/10.1001/jamaophthalmol.2016.3229
Jabs DA. Prevalence of the Uveitides in the United States. JAMA Ophthalmol. 2016;134(11):1245–6. https://doi.org/10.1001/jamaophthalmol.2016.3289
Jabs DA. Immunosuppression for the Uveitides. Ophthalmology. 2018;125(2):193–202. https://doi.org/10.1016/j.ophtha.2017.08.007
Colmán Mc Leod N. Uveítis no infecciosa y su relación con el microbioma. Rev Paraguaya Reumatol. 2022;8:53–4. https://doi.org/10.18004/rpr/2022.08.02.53
Huang XF, Brown MA. Progress in the genetics of uveitis. Genes Immun. 2022;23(2):57–65. https://doi.org/10.1038/s41435-022-00168-6
Hou S, Li N, Liao X, Kijlstra A, Yang P. Uveitis genetics. Exp Eye Res. 2020;190:107853. https://doi.org/10.1016/j.exer.2019.107853
Ambou Frutos I, Vilches Lescaille D de la C, Gómez Conde SY, Pérez Batista A, Osorio Illas L. Uveítis asociada a la artritis idiopática juvenil. Rev Cuba Oftalmol. 2021;34. URL
Takeuchi M, Mizuki N, Ohno S. Pathogenesis of Non-Infectious Uveitis Elucidated by Recent Genetic Findings. Front Immunol. 2021;12:640473. https://doi.org/10.3389/fimmu.2021.640473
Salinas Díaz MM. Presentación clínico-epidemiológico de la Uveítis en dos centros oftalmológicos de referencia del Paraguay. Discov Med. 2023;2(2):35-42. URL.
Chang JHM, Wakefield D. Uveitis: a global perspective. Ocul Immunol Inflamm. 2002;10(4):263–79. https://doi.org/10.1076/ocii.10.4.263.15592
Suhler EB, Lloyd MJ, Choi D, Rosenbaum JT, Austin DF. Incidence and Prevalence of Uveitis in Veterans Affairs Medical Centers of the Pacific Northwest. Am J Ophthalmol. 2008;146(6):890-896.e8. https://doi.org/10.1016/j.ajo.2008.09.014
Nguyen QD, Hatef E, Kayen B, Macahilig CP, Ibrahim M, Wang J, et al. A Cross-sectional Study of the Current Treatment Patterns in Noninfectious Uveitis among Specialists in the United States. Ophthalmology. 2011;118(1):184–90. https://doi.org/10.1016/j.ophtha.2010.03.029
Lopalco G, Venerito V, Sota J, Rigante D, Guerriero S, Orlando I, et al. Epidemiological profile of non-infectious uveitis from the rheumatologist’s perspective: a survey from two tertiary referral centres in Italy. Clin Exp Rheumatol. 2018;36(6 Suppl 115):68-37. URL.
McCANNEL CA, Holland GN, Helm CJ, Cornell PJ, Winston JV, Rimmer TG, et al. Causes of Uveitis in the General Practice of Ophthalmology. Am J Ophthalmol. 1996;121(1):35–46. https://doi.org/10.1016/s0002-9394(14)70532-x
Hosseini SM, Shoeibi N, Ebrahimi R, Ghasemi M. Patterns of Uveitis at a Tertiary Referral Center in Northeastern Iran. J Ophthalmic Vis Res. 2018;13(2):138–43. https://doi.org/10.4103%2Fjovr.jovr_67_17
Wakefield D, Chang JH. Epidemiology of uveitis. Int Ophthalmol Clin. 2005;45(2):1–13. https://doi.org/10.1097/01.iio.0000155938.83083.94
Joltikov KA, Lobo-Chan AM. Epidemiology and risk factors in non-infectious uveitis: a systematic review. Front Med. 2021;8:695904. https://doi.org/10.3389/fmed.2021.695904
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Abel Esteban Figueredo Rojas, Guillermo Raul Vera-Duarte, Claudia Leticia Delgado-Herrera , Martin Fernando Arrúa Caballero, Luis González Sanabria

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.