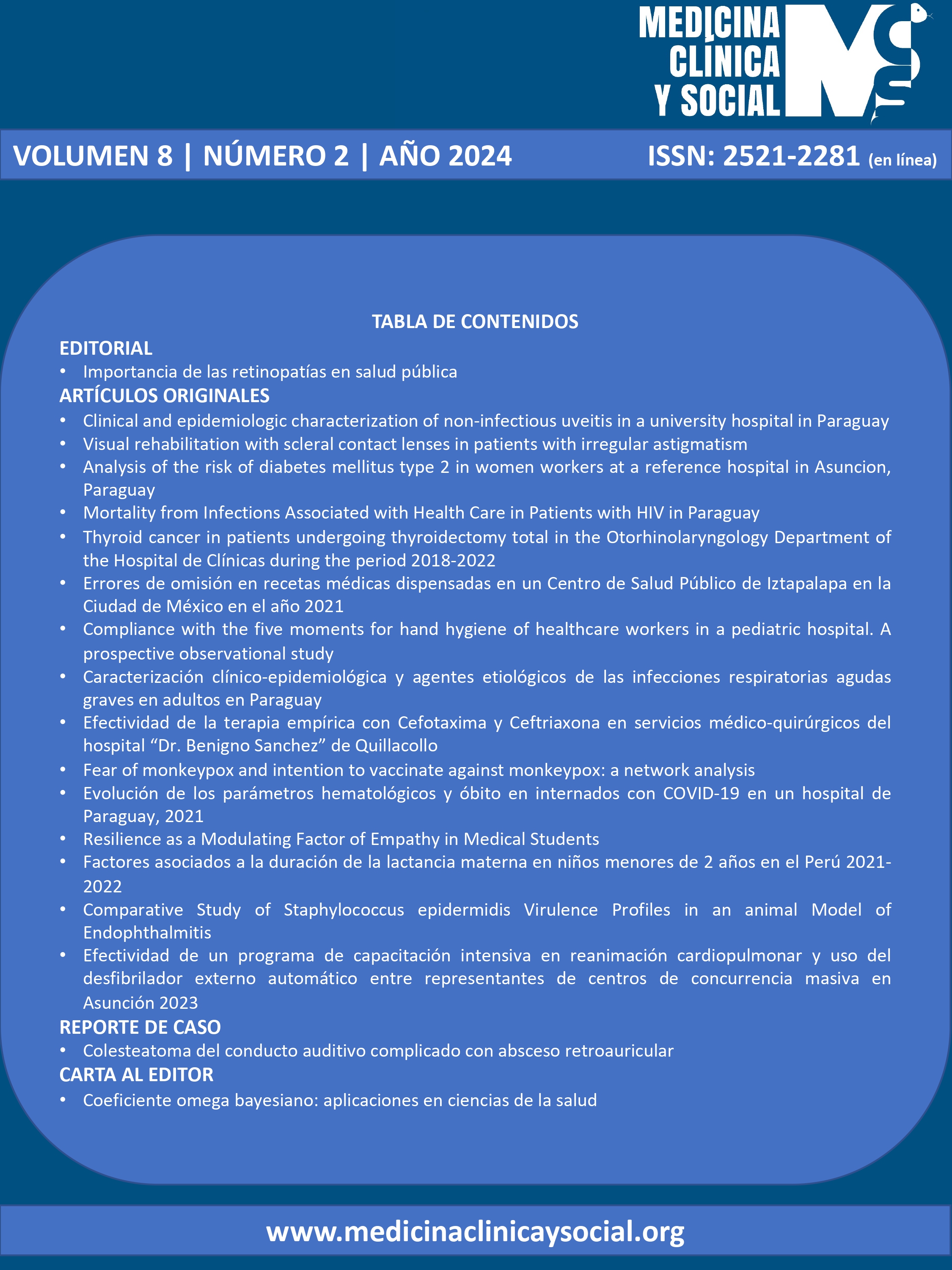
Comparative Study of Staphylococcus epidermidis Virulence Profiles in an animal Model of Endophthalmitis
DOI:
https://doi.org/10.52379/mcs.v8i2.420Palabras clave:
microbiota ocular, Staphylococcus epidermidis, modelo animal, factores de virulencia, , endoftalmitisResumen
Introduction: Gram-positive staphylococci are responsible for over 90% of cases of postoperative infectious endophthalmitis, with Staphylococcus epidermidis accounting for approximately 70% of isolated microorganisms. Objective: To evaluate the relationship between S. epidermidis virulence and severity of endophthalmitis in an animal model. Methodology: New Zealand albino rabbits were divided into two groups and administered 100 colony-forming units of S. epidermidis strains. In the virulent group, four rabbits received a multi-antibiotic resistant, mecA, ica, and atlE gene carrying S. epidermidis strain, from a patient´s conjuntival microbiota and three a biofilm-forming S. epidermidis ATCC 35984. In the non-virulent group, five rabbits were inoculated with a strain sensitive to all tested antibiotics and lacking mecA, ica, and atlE genes, also from a patient and three rabbits received the non-producer biofilm S. epidermidis ATCC 29122. Clinical and ultrasound examinations were conducted every three hours until endophthalmitis symptoms appeared, followed by daily clinical assessments. Histological evaluations were performed 15 days post-inoculation. Results: The less virulent group displayed milder inflammation and reduced intraocular damage in comparison to the more virulent group based on clinical and ultrasound observations. Nevertheless, histopathological analysis revealed similar inflammation in all groups, 15 days post-inoculation. Discussion: Less virulent S. epidermidis strains induced less severe inflammation as observed through clinical and ultrasound assessments. However, long-term histopathological assessments showed effects comparable to those seen with the more virulent strain.
Descargas
Referencias
Schwartz SG, Flynn HW Jr, Das T, Mieler WF. Ocular Infection: Endophthalmitis. Dev Ophthalmol. 2016;55:176-88. https://doi.org/10.1159/000431195
Speaker MG, Menikoff JA. Postoperative endophthalmitis: pathogenesis, prophylaxis, and management. Int Ophthalmol Clin. 1993 Winter;33(1):51-70. https://doi.org/10.1097/00004397-199303310-00006
Speaker MG, Milch FA, Shah MK, Eisner W, Kreiswirth BN. Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology. 1991 May;98(5):639-49; discussion 650. https://doi.org/10.1016/s0161-6420(91)32239-5
Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19(3):227-34. https://doi.org/10.1111/1469-0691.12118
Callegan MC, Engelbert M, Parke DW 2nd, Jett BD, Gilmore MS. Bacterial endophthalmitis: epidemiology, therapeutics, and bacterium-host interactions. Clin Microbiol Rev. 2002;15(1):111-24. https://doi.org/10.1128/cmr.15.1.111-124.2002
Callegan MC, Jett BD, Hancock LE, Gilmore MS. Role of hemolysin BL in the pathogenesis of extraintestinal Bacillus cereus infection assessed in an endophthalmitis model. Infect Immun. 1999;67(7):3357-66. https://doi.org/10.1128/iai.67.7.3357-3366.1999
Booth MC, Cheung AL, Hatter KL, Jett BD, Callegan MC, Gilmore MS. Staphylococcal accessory regulator (sar) in conjunction with agr contributes to Staphylococcus aureus virulence in endophthalmitis. Infect Immun. 1997;65(4):1550-6. https://doi.org/10.1128/iai.65.4.1550-1556.1997
Jett BD, Jensen HG, Atkuri RV, Gilmore MS. Evaluation of therapeutic measures for treating endophthalmitis caused by isogenic toxin-producing and toxin-nonproducing Enterococcus faecalis strains. Invest Ophthalmol Vis Sci. 1995;36(1):9-15. https://pubmed.ncbi.nlm.nih.gov/7822163/
Stevens SX, Jensen HG, Jett BD, Gilmore MS. A hemolysin-encoding plasmid contributes to bacterial virulence in experimental Enterococcus faecalis endophthalmitis. Invest Ophthalmol Vis Sci. 1992;33(5):1650-6. https://pubmed.ncbi.nlm.nih.gov/1559764/
Götz F. Staphylococcus and biofilms. Mol Microbiol. 2002;43(6):1367-78. https://doi.org/10.1046/j.1365-2958.2002.02827.x
McKenney D, Hübner J, Muller E, Wang Y, Goldmann DA, Pier GB. The ica locus of Staphylococcus epidermidis encodes production of the capsular polysaccharide/adhesin. Infect Immun. 1998;66(10):4711-20. https://doi.org/10.1128/iai.66.10.4711-4720.1998
Gad GF, El-Feky MA, El-Rehewy MS, Hassan MA, Abolella H, El-Baky RM. Detection of icaA, icaD genes and biofilm production by Staphylococcus aureus and Staphylococcus epidermidis isolated from urinary tract catheterized patients. J Infect Dev Ctries. 2009;3(5):342-51. https://doi.org/10.3855/jidc.241
Vandecasteele SJ, Peetermans WE, Merckx R, Van Eldere J. Expression of biofilm-associated genes in Staphylococcus epidermidis during in vitro and in vivo foreign body infections. J Infect Dis. 2003;188(5):730-7. https://doi.org/10.1086/377452
Fariña N, Carpinelli L, Samudio M, Guillén R, Laspina F, Sanabria R, et al. Clinically significant coagulase-negative staphylococci: most frequent species and virulence factors. Rev Chilena Infectol. 2013;30(5):480-8. https://doi.org/10.4067/s0716-10182013000500003
López Y, Samudio M, Fariña N, Castillo V, Abente S, Nentwich MM, González-Britez N, Laspina F, Carron A, Cibils D, de Kaspar HM. Effect of antibiotic prophylaxis on Coagulase-negative Staphylococcus virulence factor profiles in patients undergoing cataract surgery. Int Ophthalmol. 2017;37(4):929-937. https://doi.org/10.1007/s10792-016-0355-8
Fariña N, Samudio M, Carpinelli L, Nentwich MM, de Kaspar HM. Methicillin resistance and biofilm production of Staphylococcus epidermidis isolates from infectious and normal flora conjunctiva. Int Ophthalmol. 2017;37(4):819-825. https://doi.org/10.1007/s10792-016-0339-8
Astley RA, Coburn PS, Parkunan SM, Callegan MC. Modeling intraocular bacterial infections. Prog Retin Eye Res. 2016;54:30-48. https://doi.org/10.1016/j.preteyeres.2016.04.007
Miño De Kaspar H, Hoepfner AS, Engelbert M, Thiel M, Ta CN, Mette M, Schulze-Schwering M, Grasbon T, Sesma-Vea B, Casas JM, Iturralde-Goñi R, Klauss V, Kampik A. Antibiotic resistance pattern and visual outcome in experimentally-induced Staphylococcus epidermidis endophthalmitis in a rabbit model. Ophthalmology. 2001;108(3):470-8. https://doi.org/10.1016/s0161-6420(00)00545-5
Peyman GA, Paque JT, Meisels HI, Bennett TO. Postoperative endophthalmitis: a comparison of methods for treatment and prophlaxis with gentamicin. Ophthalmic Surg. 1975 Spring;6(1):45-55. URL
Ishak MA, Gröschel DH, Mandell GL, Wenzel RP. Association of slime with pathogenicity of coagulase-negative staphylococci causing nosocomial septicemia. J Clin Microbiol. 1985;22(6):1025-9. https://doi.org/10.1128/jcm.22.6.1025-1029.1985
Galdbart JO, Allignet J, Tung HS, Rydèn C, El Solh N. Screening for Staphylococcus epidermidis markers discriminating between skin-flora strains and those responsible for infections of joint prostheses. J Infect Dis. 2000;182(1):351-5. https://doi.org/10.1086/315660
Klingenberg C, Aarag E, Rønnestad A, Sollid JE, Abrahamsen TG, Kjeldsen G, Flaegstad T. Coagulase-negative staphylococcal sepsis in neonates. Association between antibiotic resistance, biofilm formation and the host inflammatory response. Pediatr Infect Dis J. 2005;24(9):817-22. https://doi.org/10.1097/01.inf.0000176735.20008.cd
Das S, Singh S, Kumar A. Bacterial Burden Declines But Neutrophil Infiltration and Ocular Tissue Damage Persist in Experimental Staphylococcus epidermidis Endophthalmitis. Front Cell Infect Microbiol. 2021 17;11:780648. https://doi.org/10.3389/fcimb.2021.780648
Meredith TA, Trabelsi A, Miller MJ, Aguilar E, Wilson LA. Spontaneous sterilization in experimental Staphylococcus epidermidis endophthalmitis. Invest Ophthalmol Vis Sci. 1990;31(1):181-6. URL
Li B, Miño de Kaspar H, Haritoglou C, Kook D, Kampik A, Sheng M, Nentwich MM. Comparison of 1-day versus 1-hour application of topical neomycin/polymyxin-B before cataract surgery. J Cataract Refract Surg. 2015;41(4):724-31. https://doi.org/10.1016/j.jcrs.2014.06.042
Nentwich MM, Rajab M, Ta CN, He L, Grueterich M, Haritoglou C, Gandorfer A, Kampik A, Mino De Kaspar H. Application of 10% povidone iodine reduces conjunctival bacterial contamination rate in patients undergoing cataract surgery. Eur J Ophthalmol. 2012;22(4):541-6. https://doi.org/10.5301/ejo.5000093
Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone-iodine. Ophthalmology. 1991;98(12):1769-75. https://doi.org/10.1016/s0161-6420(91)32052-9
Nentwich MM, Yactayo-Miranda Y, Schwarzbach F, Wolf A, Kampik A, Mino de Kaspar H. Endophthalmitis after intravitreal injection: decreasing incidence and clinical outcome-8-year results from a tertiary ophthalmic referral center. Retina. 2014;34(5):943-50. https://doi.org/10.1097/iae.0000000000000011
Nentwich MM, Ta CN, Kreutzer TC, Li B, Schwarzbach F, Yactayo-Miranda YM, Kampik A, Miño de Kaspar H. Incidence of postoperative endophthalmitis from 1990 to 2009 using povidone-iodine but no intracameral antibiotics at a single academic institution. J Cataract Refract Surg. 2015;41(1):58-66. https://doi.org/10.1016/j.jcrs.2014.04.040
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Margarita Samudio, Sonia Abente, Vanesa Villalba, Jason Penniecook, Emilio González, Alicia Schinini, Susy Figueredo, Carolina Duré, Herminia Mino de Kaspar

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.