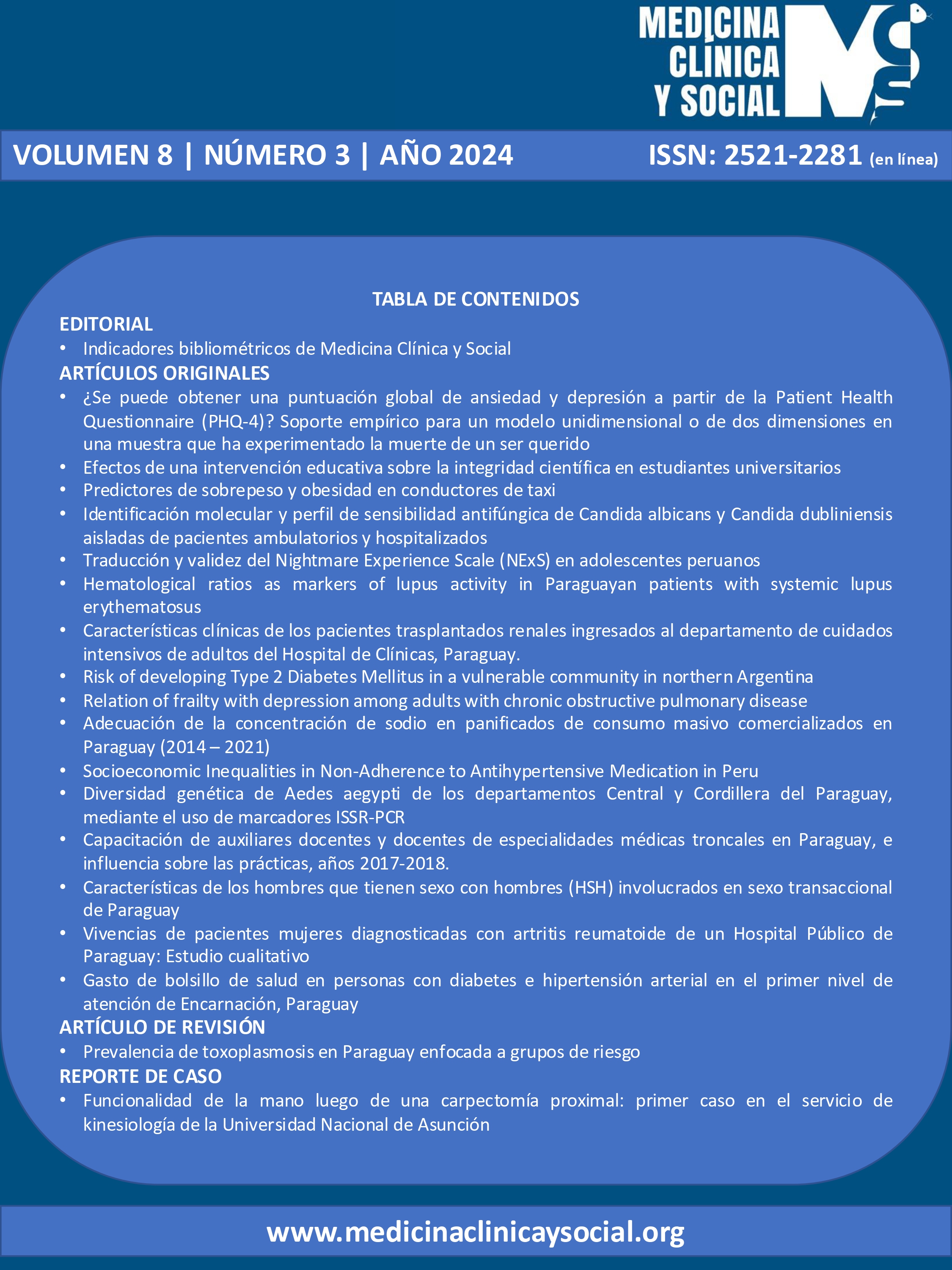
Hematological ratios as markers of lupus activity in Paraguayan patients with systemic lupus erythematosus
DOI:
https://doi.org/10.52379/mcs.v8i3.437Palabras clave:
Systemic lupus erythematosus (SLE), Neutrophil/lymphocyte ratio, Platelet/lymphocyte ratio, Eosinophil/lymphocyte ratio, Monocyte/Lymphocyte ratioResumen
Introduction: The neutrophil/lymphocyte ratio (NLR) and the platelet/lymphocyte ratio (PLR) are markers of inflammation and prognosis in systemic diseases. This study determined the association between hematological indices, and disease activity in patients with systemic lupus erythematosus (SLE). Methods: This prospective, observational and analytical cross-sectional study included 87 Paraguayan patients diagnosed with SLE, according to the ACR/EULAR 2019 criteria. We investigate four hematological indices: neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio (PLR), eosinophil/lymphocyte ratio (ELR), and monocytes/lymphocyte ratio (MLR). Results: Eighty-seven percent were female, with a median age of 34.9 ±12.3 years. SLEDAI mean of 3.68 ± 4.76 was found. SLEDAI mean was 3.68 ± 4.76. Positivity of anti-DNAds was found in 52% of the patients. CRP mean was 3.5 ± 4.6. Regarding values of hematological indices, we found: NLR mean of 2.4 ± 1.6 was obtained, ELR 0.07 ± 0.09, MRL 0.07 ± 0.07 and PLR 155.89 ± 80.69. A significant positive correlation was found with SLEDAI and NLR (r=0.34, p=0.001). Based on the ROC curve, the best cut-off value for our patient cohort capable of predicting patients with high activity is for NLR values ? 2.283 (AUC: 0.66). Conclusion: NLR could be a valuable and accessible biomarker to identify elevated activity in patients with SLE.
Descargas
Referencias
REFERENCES
Rebak J, Yucra D, Brigante J, Hamaui A, Dubinsky D. Neutropenia al diagno?stico de lupus eritematoso siste?mico: prevalencia y correlaciones cli?nicas y serolo?gicas: Nuestra cohorte. Rev. Argent. Reumatol. 2022;33(2):76 -82. https://doi.org/10.47196/rar.v33i2.609
Kandane-Rathnayake R, Louthrenoo W, Golder V, Luo SF, Wu YJJ, Lateef A, & Asia Pacific Lupus Collaboration. Independent associations of lymphopenia and neutropenia in patients with systemic lupus erythematosus: a longitudinal, multinational study. Rheumatology.2021; 60(11):5185-5193. https://doi.org/10.1093/rheumatology/keab217
Carli L, Tani C, Vagnani S, Signorini V, Mosca M. Leukopenia, lymphopenia, and neutropenia in systemic lupus erythematosus: Prevalence and clinical impact--A systematic literature review. Semin Arthritis Rheum. 2015;45(2):190-194. https://doi.org/10.1016/j.semarthrit.2015.05.009
Rivero SJ, Díaz-Jouanen E, Alarcón-Segovia D. Lymphopenia in systemic lupus erythematosus. Clinical, diagnostic, and prognostic significance. Arthritis Rheum. 1978;21(3):295-305. https://doi.org/10.1002/art.1780210302
Liu J, Ao W, Zhou J, Luo P, Wang Q, Xiang D. The correlation between PLR-NLR and prognosis in acute myocardial infarction. Am J Transl Res. 2021;13(5):4892-4899. URL
Maravilla Domínguez MA, Zermeño González ML, Zavaleta Muñiz ER, Montes Varela VA, Irecta Nájera CA, Fajardo Robledo NS, et al. Inflammation and atherogenic markers in patients with type 2 diabetes mellitus. Clin Investig Arterioscler. 2022;34(3):105-112. https://doi.org/10.1016/j.arteri.2021.03.006
Feng JF, Huang Y, Chen QX. Preoperative platelet lymphocyte ratio (PLR) is superior to neutrophil lymphocyte ratio (NLR) as a predictive factor in patients with esophageal squamous cell carcinoma. World J Surg Oncol. 2014;12:58. https://doi.org/10.1186/1477-7819-12-58
Erre GL, Paliogiannis P, Castagna F, Mangoni AA, Carru C, Passiu G, et al. Meta-analysis of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in rheumatoid arthritis. Eur J Clin Invest. 2019;49(1):e13037. https://doi.org/10.1111/eci.13037
Qin B, Ma N, Tang Q, Wei T, Yang M, Fu H, et al. Neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) were useful markers in assessment of inflammatory response and disease activity in SLE patients. Mod Rheumatol. 2016;26(3):372-6. https://doi.org/10.3109/14397595.2015.1091136
Suszek D, Górak A, Majdan M. Differential approach to peripheral blood cell ratios in patients with systemic lupus erythematosus and various manifestations. Rheumatol Int. 2020;40(10):1625-1629. https://doi.org/10.1007/s00296-020-04669-3
Wang L, Wang C, Jia X, Yang M, Yu J. Relationship between Neutrophil-to-Lymphocyte Ratio and Systemic Lupus Erythematosus: A Meta-analysis. Clinics (Sao Paulo). 2020;75:e1450. https://doi.org/10.6061/clinics/2020/e1450
Yu J, Zeng T, Wu Y, Tian Y, Tan L, Duan X, et al. Neutrophil-to-C3 ratio and neutrophil-to-lymphocyte ratio were associated with disease activity in patients with systemic lupus erythematosus. J Clin Lab Anal. 2019;33(1):e22633. https://doi.org/10.1002/jcla.22633
Ma L, Zeng A, Chen B, Chen Y, Zhou R. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in patients with systemic lupus erythematosus and their correlation with activity: A meta-analysis. Int Immunopharmacol. 2019;76:105949. https://doi.org/10.1016/j.intimp.2019.105949
Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The Platelet-to-Lymphocyte Ratio as an Inflammatory Marker in Rheumatic Diseases. Ann Lab Med. 2019;39(4):345-357. https://doi.org/10.3343/alm.2019.39.4.345
Hao X, Li D, Wu D, Zhang N. The Relationship between Hematological Indices and Autoimmune Rheumatic Diseases (ARDs), a Meta-Analysis. Sci Rep. 2017;7(1):10833. https://doi.org/10.1038/s41598-017-11398-4
Maharani W, Ratnaningsih DF, Utami F, Yulianto FA, Dewina A, Hamijoyo L, Atik N. Activity Disease in SLE Patients Affected IFN-? in the IGRA Results. J Inflamm Res. 2020;13:433-439. https://doi.org/10.2147/jir.s258235
Ramirez GA, Manfredi AA, Maugeri N. Misunderstandings Between Platelets and Neutrophils Build in Chronic Inflammation. Front Immunol. 2019;10:2491. https://doi.org/10.3389/fimmu.2019.02491
Firizal AS, Sugianli AK, Hamijoyo L. Cut off point of neutrophil-to-lymphocyte ratio as a marker of active disease in systemic lupus erythematosus. Lupus. 2020;29(12):1566-1570. https://doi.org/10.1177/0961203320950822
Wu Y, Chen Y, Yang X, Chen L, Yang Y. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were associated with disease activity in patients with systemic lupus erythematosus. Int Immunopharmacol. 2016;36:94-9. https://doi.org/10.1016/j.intimp.2016.04.006
Li W, Liu S, Chen C, Han Y. Neutrophil-to-lymphocyte ratios and platelet-to-lymphocyte ratios in juvenile systemic lupus erythematosus: correlation with disease manifestations. Ann Palliat Med. 2021;10(9):9406-9414. https://doi.org/10.21037/apm-21-1995
Yang Z, Zhang Z, Lin F, Ren Y, Liu D, Zhong R, Liang Y. Comparisons of neutrophil-, monocyte-, eosinophil-, and basophil- lymphocyte ratios among various systemic autoimmune rheumatic diseases. APMIS. 2017;125(10):863-871. https://doi.org/10.1111/apm.12722
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Zoilo Morel, Rodrigo Acosta, Astrid Paats, Sonia Cabrera Villalba, Paloma de Abreu, Gabriela Avila Pedretti, Osmar Antonio Centurion, María Eugenia Acosta, María Teresa Martinez de Filartiga, Yurilis Fuentes Silva, Isabel Acosta Colman

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.