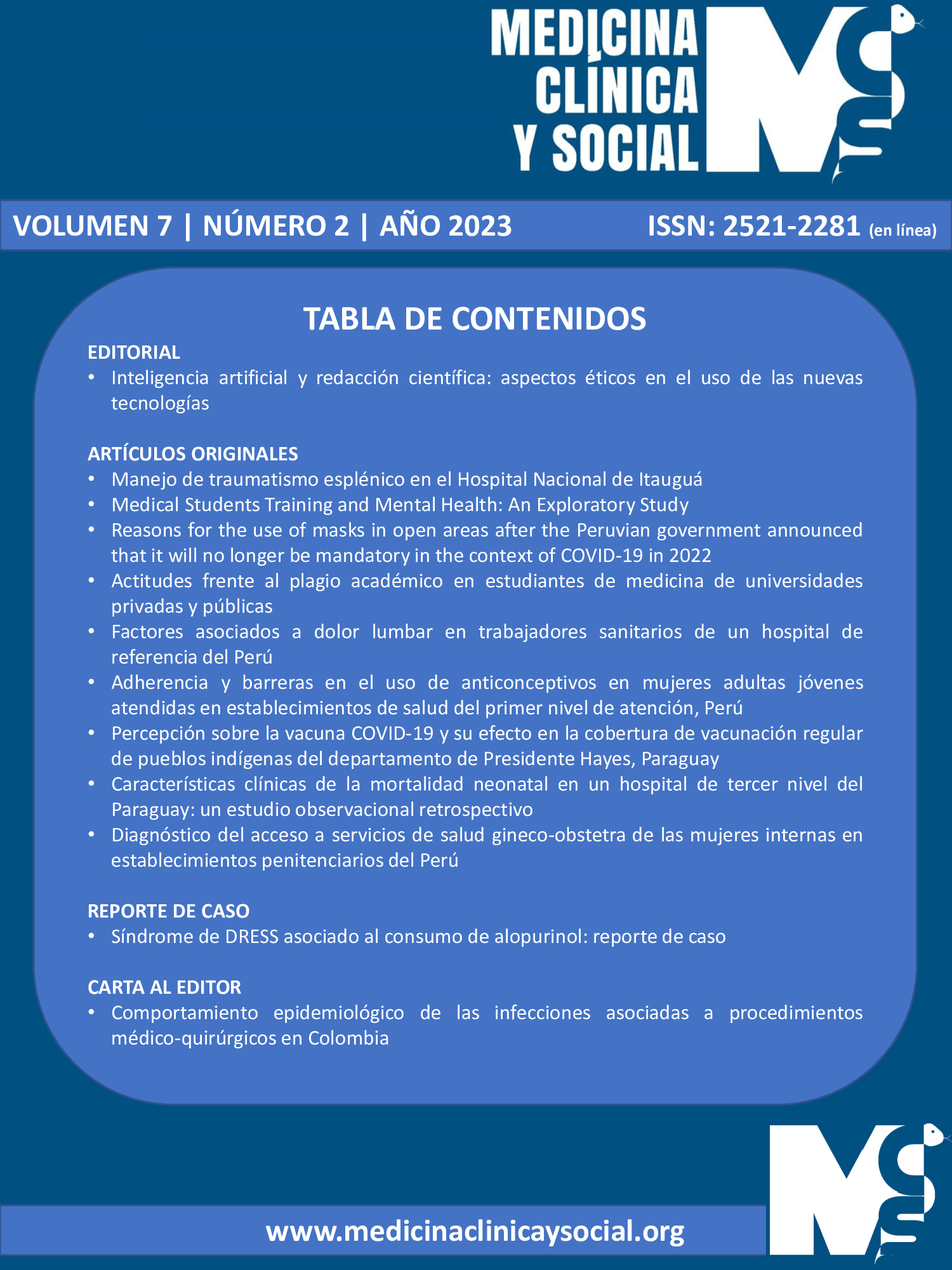
Clinical characteristics of neonatal mortality in a tertiary level hospital in Paraguay: a retrospective observational study.
DOI:
https://doi.org/10.52379/mcs.v7i2.294Keywords:
Early Neonatal Mortality, Comorbidity, Infant, Newborn, DiseasesAbstract
Introduction: Neonatal mortality remains a major public health problem worldwide, particularly in developing countries. Most neonatal deaths are attributable to preventable complications, such as premature birth, neonatal sepsis, and birth asphyxia. Objective: To determine the clinical characteristics of neonatal mortality in a tertiary-level hospital in Paraguay through a retrospective observational study. Methods: This observational, descriptive, and retrospective study was conducted at the Hospital de Clínicas in Paraguay. This design allowed information to be obtained from the medical records of newborns who attended the hospital over a period of five years. Results: Between 2018 and 2022, 121 cases of neonatal mortality were recorded at the Hospital de Clínicas del Paraguay. The mean birth weight was 2013.51 ± 1021 kg and mean gestational age was 32.87 ± 4.6 weeks. The most frequent diagnoses of neonatal death were sepsis (37 cases), cardiac involvement (61 cases), and genetic syndromes (39 cases). Discussion: The data obtained from this study suggest that maternal and neonatal risk factors are associated with neonatal mortality in the Hospital de Clínicas of Paraguay. Further studies are needed to analyze these factors and develop preventive strategies to reduce the neonatal mortality rate in the country
Downloads
References
Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-Saharan Africa: A systematic review and meta-analysis. PLOS ONE. 2019;14(9):e0222566. https://doi.org/10.1371%2Fjournal.pone.0222566
Orsido TT, Asseffa NA, Berheto TM. Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):83. https://doi.org/10.1186/s12884-019-2227-5
Andegiorgish AK, Andemariam M, Temesghen S, Ogbai L, Ogbe Z, Zeng L. Neonatal mortality and associated factors in the specialized neonatal care unit Asmara, Eritrea. BMC Public Health. 2020;20(1):10. https://doi.org/10.1186/s12889-019-8118-x
Chou VB, Walker N, Kanyangarara M. Estimating the global impact of poor quality of care on maternal and neonatal outcomes in 81 low- and middle-income countries: A modeling study. PLOS Medicine. 2019;16(12):e1002990. https://doi.org/10.1371/journal.pmed.1002990
Veloso FCS, Kassar L de ML, Oliveira MJC, Lima THB de, Bueno NB, Gurgel RQ, et al. Analysis of neonatal mortality risk factors in Brazil: a systematic review and meta-analysis of observational studies. J Pediatr (Rio J). 2019;95:519-30. https://doi.org/10.1016/j.jped.2018.12.014
Al-Sheyab NA, Khader YS, Shattnawi KK, Alyahya MS, Batieha A. Rate, Risk Factors, and Causes of Neonatal Deaths in Jordan: Analysis of Data From Jordan Stillbirth and Neonatal Surveillance System (JSANDS). Frontiers in Public Health. 2020;8. https://doi.org/10.3389/fpubh.2020.595379
Vilanova CS, Hirakata VN, de Souza Buriol VC, Nunes M, Goldani MZ, da Silva CH. The relationship between the different low birth weight strata of newborns with infant mortality and the influence of the main health determinants in the extreme south of Brazil. Population Health Metrics. 2019;17(1):15. https://doi.org/10.1186/s12963-019-0195-7
Wang L, Tang S, Liu H, Ma J, Li B, Wu L, et al. The Underlying Causes of Respiratory Distress in Late-Preterm and Full-Term Infants Are Different From Those of Early-Preterm Infants. Innov J Pediatr. 2020;30(5):e104011. https://doi.org/10.5812/ijp.104011
Muglu J, Rather H, Arroyo-Manzano D, Bhattacharya S, Balchin I, Khalil A, et al. Risks of stillbirth and neonatal death with advancing gestation at term: A systematic review and meta-analysis of cohort studies of 15 million pregnancies. PLOS Medicine. 2019;16(7):e1002838. https://doi.org/10.1371/journal.pmed.1002838
Kunkel M, Marete I, Cheng ER, Bucher S, Liechty E, Esamai F, et al. Place of delivery and perinatal mortality in Kenya. Seminars in Perinatology. 2019;43(5):252-9. https://doi.org/10.1053/j.semperi.2019.03.014
Zhang X, Bai L, Ren H, Liu X, Guo S, Xu P, et al. Perinatal and maternal outcomes after frozen versus fresh embryo transfer cycles in women of advanced maternal age. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2021;257:133-7. https://doi.org/10.1016/j.ejogrb.2020.09.047
Kim SY, Park JY, Bak SE, Jang YR, Wie JH, Ko HS, et al. Effect of maternal age on emergency cesarean section. The Journal of Maternal-Fetal & Neonatal Medicine. 2020;33(23):3969-76. https://doi.org/10.1080/14767058.2019.1593958
Marecos PE, Duarte C, Sanabria LM. Causas más frecuentes de mortalidad en recién nacidos prematuros, registradas en un hospital materno infantil de la ciudad de Asunción-Paraguay. Revista Científica Estudios e Investigaciones. 2014;3(1):237-50. URL.
Tumas N, Godoy AC, Peresini V, Peisino ME, Boldrini G, Vaggione G, et al. El cuidado prenatal y los determinantes sociales: estudio ecológico en Argentina. Población y Salud en Mesoamérica. 2022;19(2):224-44. https://doi.org/10.15517/psm.v0i19.47439
Vester JM, Delgadillo L. Morbimortalidad infantil en pacientes hospitalizados en un hospital de referencia. Paraguay 2018. Revista científica ciencias de la salud. 2021;3(2):69-77. https://doi.org/10.53732/rccsalud/03.02.2021.69
Bitew ZW, Alemu A, Ayele EG, Jember DA, Haile MT, Worku T. Incidence Density Rate of Neonatal Mortality and Predictors in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. International Journal of Pediatrics. 2020;2020:e3894026. https://doi.org/10.1155/2020/3894026
Mangu CD, Rumisha SF, Lyimo EP, Mremi IR, Massawe IS, Bwana VM, et al. Trends, patterns and cause-specific neonatal mortality in Tanzania: a hospital-based retrospective survey. International Health. 2021;13(4):334-43. https://doi.org/10.1093/inthealth/ihaa070
Mohamed HA, Shiferaw Z, Roble AK, Kure MA. Neonatal mortality and associated factors among neonates admitted to neonatal intensive care unit at public hospitals of Somali Regional State, Eastern Ethiopia: A multicenter retrospective analysis. PLoS One. 2022;17(5):e0268648. https://doi.org/10.1186/s12889-019-8118-x
Taksande A, Jameel PZ. Critical Congenital Heart Disease in Neonates: A Review Article. Current Pediatric Reviews. 2021;17(2):120–6. https://doi.org/10.2174/1573396317666210219162515
Jamali Z, Sinaei R, Razi L. Multisystem Inflammatory Syndrome in a Newborn (MIS-N): Clinical Evidence and Neurodevelopmental Outcome. Current Pediatric Reviews. 2023;19(2):210-2. https://doi.org/10.2174/1573396318666220806143047
Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, et al. Assessment of Neonatal Intensive Care Unit Practices, Morbidity, and Mortality Among Very Preterm Infants in China. JAMA Network Open. 2021;4(8):e2118904. https://doi.org/10.1001/jamanetworkopen.2021.18904
Abd El Aziz T, Elbanna E, Sarhan D, Ibrahim SE. Clinical Characterizations of Neonatal Admission in Neonatal Intensive Care Unit at Zagazig University Children Hospital. Zagazig University Medical Journal. 2020;26(5):775-86. https://doi.org/10.21608/zumj.2019.16984.1519
Al-Momani MM. Admission patterns and risk factors linked with neonatal mortality: A hospital-based retrospective study. Pak J Med Sci. 2020;36(6):1371-6. https://doi.org/10.12669%2Fpjms.36.6.2281
Yismaw AE, Gelagay AA, Sisay MM. Survival and predictors among preterm neonates admitted at University of Gondar comprehensive specialized hospital neonatal intensive care unit, Northwest Ethiopia. Ital J Pediatr. 2019;45(1):4. https://doi.org/10.1186/s13052-018-0597-3
Peters L, Olson L, Khu DTK, Linnros S, Le NK, Hanberger H, et al. Multiple antibiotic resistance as a risk factor for mortality and prolonged hospital stay: A cohort study among neonatal intensive care patients with hospital-acquired infections caused by gram-negative bacteria in Vietnam. PLOS ONE. 2019;14(5):e0215666. https://doi.org/10.1371/journal.pone.0215666
Seid SS, Ibro SA, Ahmed AA, Olani Akuma A, Reta EY, Haso TK, et al. Causes and factors associated with neonatal mortality in Neonatal Intensive Care Unit (NICU) of Jimma University Medical Center, Jimma, South West Ethiopia. Pediatric Health, Medicine and Therapeutics. 2019;10:39-48. https://doi.org/10.2147/phmt.s197280
Puri A, Lal B, Nangia S. A Pilot Study on Neonatal Surgical Mortality: A Multivariable Analysis of Predictors of Mortality in a Resource-Limited Setting. J Indian Assoc Pediatr Surg. 2019;24(1):36-44. https://doi.org/10.4103%2Fjiaps.JIAPS_30_18
Downloads
Published
Issue
Section
License
Copyright (c) 2023 Cielos Jemima Cantero Noguera, Deisy Beatriz Colmán Gómez, Shirley Rocío Oviedo Ramírez, Alba María Cordone Ramos

This work is licensed under a Creative Commons Attribution 4.0 International License.