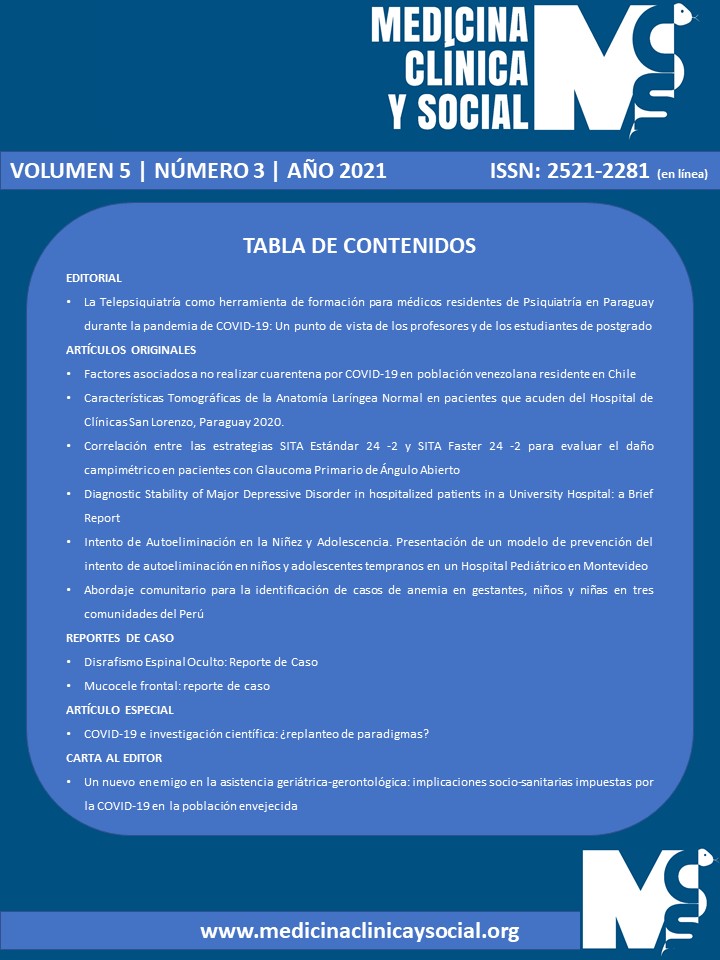
Diagnostic Stability of Major Depressive Disorder in hospitalized patients in a University Hospital: a Brief Report
DOI:
https://doi.org/10.52379/mcs.v5i3.223Palabras clave:
diagnóstico, estabilidad diagnóstica, trastorno depresivo mayor, trastorno límite de la personalidadResumen
Introduction: There may be a discordance between diagnoses at admission and discharge of mentally ill patients with major issues regarding their diagnostic stability. The objective of this brief report was to determine the diagnostic stability of major depressive disorder at patients’ discharge and if the diagnosis of their hospital admission had been retained. Methodology: This was a pilot, descriptive, cross-sectional, and retrospective observational study. A non-probabilistic sampling of consecutive cases was used. We reviewed the medical records, at admission and discharge, of patients with an initial diagnosis of major depressive disorder, hospitalized in the Department of Psychiatry of the ‘Hospital de Clínicas’ of the National University of Asunción, Paraguay, during the months of October to December 2020. Results: Fifty-three patients with a diagnosis of major depression on their hospital admission were included in the study (mean age = 35.7 ± 16.5 years). 79.2 % were women, 52.8 % were single, and 37.7 % were from the Central province of Paraguay. The most frequent diagnosis at discharge was borderline personality disorder, in 35.8% of cases. Major depressive disorder was confirmed in 15.1% of cases. No significant relationship was found between any discharge diagnosis and sociodemographic data. Conclusion: The results of this study, although preliminary, described the trajectories of diagnoses in the Psychiatry Department of a University hospital, but confirmatory studies are needed.
Descargas
Referencias
Cui R. Editorial: A Systematic Review of Depression. Curr Neuropharmacol. 2015;13(4):480. https://doi.org/10.2174/1570159x1304150831123535
Torales J, Ventriglio A, Barrios I, Arce A. Demographic and clinical characteristics of patients referred to the psychiatry unit of the emergency department at the National University of Asunción’s General Hospital, Paraguay. Int J Cult Ment Health. 2016;9(3):233-238. https://doi.org/10.1080/17542863.2016.1197290
Melgarejo OJ, Torales JC, Cantero JB. Código Z: necesidad de integrar un trabajador social psiquiátrico a la sala de internación del Servicio de Psiquiatría del Hospital de Clínicas. Un estudio piloto. An. Fac. Cien. Méd. (Asunción) 2017;50(3):29-40. https://doi.org/10.18004/anales/2017.050(03)29-040
Sánchez R, Jaramillo LE, Quintero C. Estabilidad del Diagnóstico Psiquiátrico en Pacientes de Consulta Externa. Rev Colomb Psiquiatr. 2002;31(2):101-122. URL.
Kendell RE. The stability of psychiatric diagnosis. Br J Psychiatry. 1974;124(0):352-356. https://doi.org/10.1192/bjp.124.4.352
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington VA. APA Press, 2013.
Muñoz Navarro SR. ¿Cuántos sujetos necesito para mi estudio? [How many subjects do I need to power my study?]. Medwave. 2014;14(6):e5995. https://doi.org/10.5867/medwave.2014.06.5995
Cegla-Schvartzman FB, Ovejero S, López-Castroman J, Baca-García E. Diagnostic Stability in Bipolar Disorder: A Narrative Review. Harv Rev Psychiatry. 2019;27(1):3-14. https://doi.org/10.1097/HRP.0000000000000187
Paris J. Differential Diagnosis of Borderline Personality Disorder. Psychiatr Clin North Am. 2018;41(4):575-582. https://doi.org/10.1016/j.psc.2018.07.001
Rao S, Broadbear J. Borderline personality disorder and depressive disorder. Australas Psychiatry. 2019;27(6):573-577. https://doi.org/10.1177/1039856219878643
Beatson JA, Rao S. Depression and borderline personality disorder. Med J Aust 2013; 199(6):S24-S27. https://doi.org/10.5694/mja12.10474
Kjær JN, Biskin R, Vestergaard C, Gustafsson LN, Munk-Jørgensen P. The clinical trajectory of patients with borderline personality disorder. Personality and Mental Health 2016;10:181-190. https://doi.org/10.1002/pmh.1337
Blázquez A, Ortiz AE, Castro-Fornieles J, Morer A, Baeza I, Martínez E, et al. Five-year diagnostic stability among adolescents in an inpatient psychiatric unit. Comprehensive Psychiatry 2019;89:33-39. https://doi.org/10.1016/j.comppsych.2018.11.011
Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, et al. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017;135(4):273-284. https://doi.org/10.1111/acps.12686
Chen MH, Chen YS, Hsu JW, Huang KL, Li CT, Lin WC, et al. Comorbidity of ADHD and subsequent bipolar disorder among adolescents and young adults with major depression: a nationwide longitudinal study. Bipolar Disord. 2015;17(3):315-322. https://doi.org/10.1111/bdi.12266
Bukh JD, Andersen PK, Kessing LV. Rates and predictors of remission, recurrence and conversion to bipolar disorder after the first lifetime episode of depression--a prospective 5-year follow-up study. Psychol Med. 2016;46(6):1151-1161. https://doi.org/10.1017/S0033291715002676
Kessing LV. Diagnostic stability in depressive disorder as according to ICD-10 in clinical practice. Psychopathology. 2005;38(1):32-37. https://doi.org/10.1159/000083968
Schwartz JE, Fennig S, Tanenberg-Karant M, Carlson G, Craig T, Galambos N, et al. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry. 2000;57(6):593-600. https://doi.org/10.1001/archpsyc.57.6.593
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2021 Enrique De Doménico, João Mauricio Castaldelli-Maia, Antonio Ventriglio, Julio Torales

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.