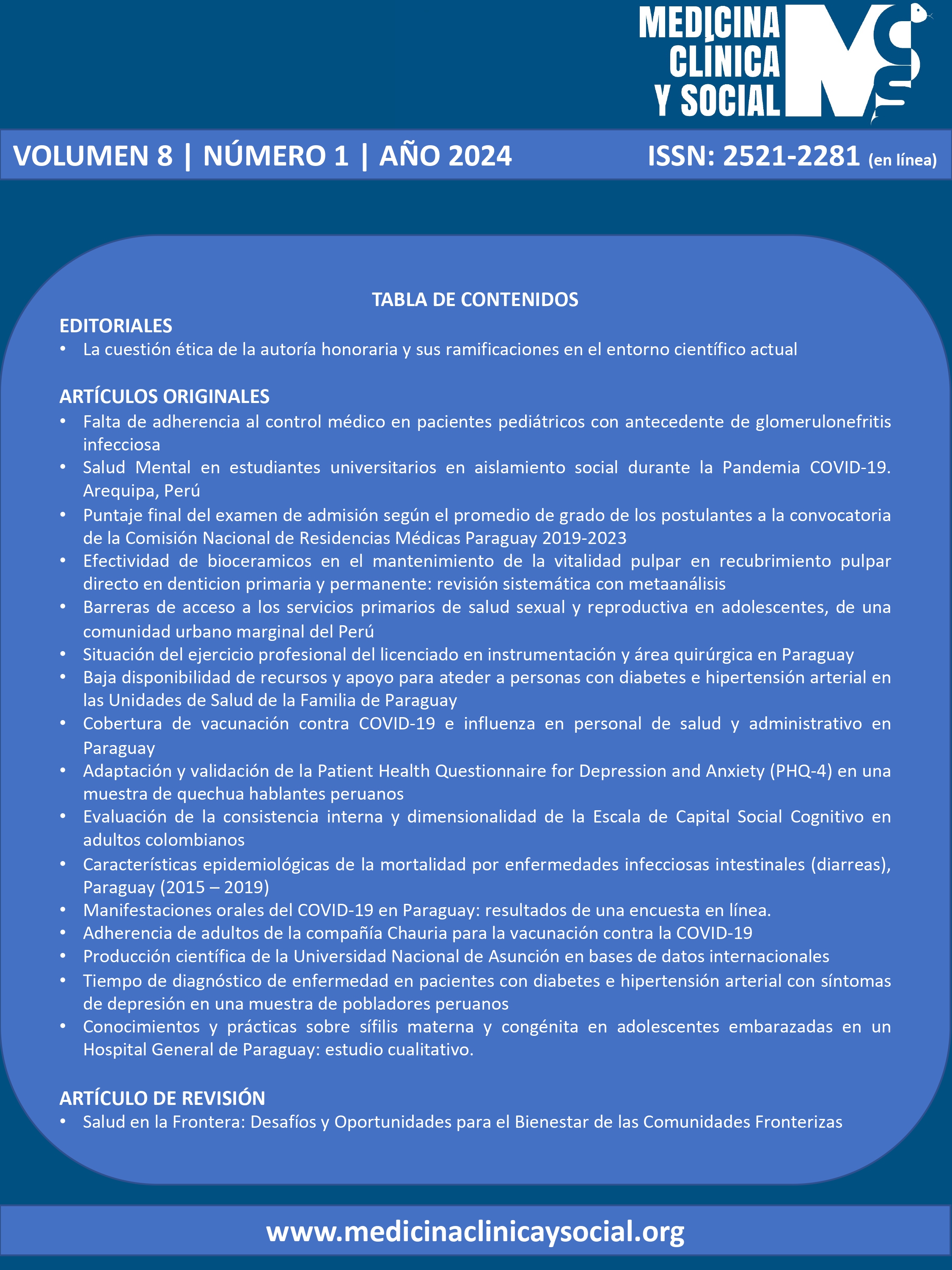
Salud en la Frontera: Desafíos y Oportunidades para el Bienestar de las Comunidades Fronterizas
DOI:
https://doi.org/10.52379/mcs.v8i1.323Palabras clave:
Salud Pública, Medio ambiente, Medicina preventinva y Salud Pública, Pluriculturalismo, FronteraResumen
La salud en la frontera presenta una serie de desafíos y oportunidades para el bienestar de las comunidades fronterizas. Estas zonas geográficas, donde los límites políticos y territoriales se entrelazan, enfrentan problemas de salud únicos que requieren enfoques innovadores y colaborativos. Uno de los desafíos principales es el acceso limitado a servicios de atención médica de calidad. Las comunidades fronterizas a menudo carecen de infraestructuras de salud adecuadas, incluyendo hospitales y clínicas, lo que dificulta el acceso a servicios esenciales. Además, las barreras lingüísticas y culturales pueden dificultar aún más la comunicación entre los proveedores de salud y los pacientes, lo que limita la calidad de la atención. A pesar de estos desafíos, también existen oportunidades para mejorar la salud en la frontera. La colaboración transfronteriza puede ser una herramienta poderosa para abordar los problemas de salud comunes. Los países vecinos pueden compartir recursos, conocimientos y mejores prácticas para fortalecer los sistemas de salud en ambos lados de la frontera. Esto incluye la promoción de la formación y capacitación conjunta de profesionales de la salud, el intercambio de información epidemiológica y la armonización de políticas de salud. Además, las comunidades fronterizas pueden aprovechar su diversidad cultural y su conocimiento tradicional para mejorar la atención médica.
Descargas
Referencias
Logan RI, Castañeda H. Addressing Health Disparities in the Rural United States: Advocacy as Caregiving among Community Health Workers and Promotores de Salud. Int J Environ Res Public Health. 2020;17(24):9223. https://doi.org/10.3390/ijerph17249223.
Lichter D.T. Immigration and the new racial diversity in rural America. Rural Sociol. 2012;77:3–35. https://doi.org/10.1111/j.1549-0831.2012.00070.x
Carrillo G, Uribe F, Lucio R, Ramirez Lopez A, Korc M. The United States-Mexico border environmental public health: the challenges of working with two systems. Rev Panam Salud Publica. 2017;41:e98. https://doi.org/10.26633/RPSP.2017.98
Nittari G, Khuman R, Baldoni S, Pallotta G, Battineni G, Sirignano A, et al. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed J E Health. 2020;26(12):1427-1437. https://doi.org/10.1089/tmj.2019.0158
Saldanha R, Mosnier É, Barcellos C, Carbunar A, Charron C, Desconnets JC, et al. Contributing to Elimination of Cross-Border Malaria Through a Standardized Solution for Case Surveillance, Data Sharing, and Data Interpretation: Development of a Cross-Border Monitoring System. JMIR Public Health Surveill. 2020;6(3):e15409. https://doi.org/10.2196/15409
George J, Häsler B, Mremi I, Sindato C, Mboera L, Rweyemamu M, et al. A systematic review on integration mechanisms in human and animal health surveillance systems with a view to addressing global health security threats. One Health Outlook. 2020;2:11. https://doi.org/10.1186/s42522-020-00017-4
Gao Q, Liu Y, Ayub B, Hussain M. Does Health Crises Effect Tourism: Role of Financial Inclusion for Green Financial Development. Front Public Health. 2022;10:896894. https://doi.org/10.3389/fpubh.2022.896894
Lee K, Grépin KA, Worsnop C, Marion S, Piper J, Song M. Managing borders during public health emergencies of international concern: a proposed typology of cross-border health measures. Global Health. 2021;17(1):62. https://doi.org/10.1186/s12992-021-00709-0
Asai Y. Assessing the efficacy of health countermeasures on arrival time of infectious diseases. Infect Dis Model. 2023;8(2):603-616. https://doi.org/10.1016/j.idm.2023.05.004
Martinez-Donate AP, Verdecias N, Zhang X, Jesús Eduardo GF, Asadi-Gonzalez AA, Guendelman S, Amuedo-Dorantes C, Rangel G. Health Profile and Health Care Access of Mexican Migration Flows Traversing the Northern Border of Mexico. Med Care. 2020;58(5):474-482. https://doi.org/10.1097/MLR.0000000000001300
Dilger H, Mattes D. Im/mobilities and dis/connectivities in medical globalisation: How global is Global Health? Glob Public Health. 2018;13(3):265-275. https://doi.org/10.1080/17441692.2017.1414285
Munch A, Verhaegh B. Cross-border scientific projects run by UEG national member societies reduce health inequalities across Europe. United European Gastroenterol J. 2016;4(3):478. https://doi.org/10.1177/2050640616651200 m
Quinn SC, Kumar S. Health inequalities and infectious disease epidemics: a challenge for global health security. Biosecur Bioterror. 2014;12(5):263-73. https://doi.org/10.1089/bsp.2014.0032
Cerqueira MT. Health and human security in border regions. Rev Panam Salud Publica. 2012;31(5):362-4, 359-61. https://doi.org/10.1590/s1020-49892012000500002
Daniel C, Ouagne D, Sadou E, Paris N, Hussain S, Jaulent MC, et al. Cross border semantic interoperability for learning health systems: The EHR4CR semantic resources and services. Learn Health Syst. 2016;1(1):e10014. https://doi.org/10.1002/lrh2.10014
Levino A, Carvalho EF. Análise comparativa dos sistemas de saúde da tríplice fronteira: Brasil/Colômbia/Peru. Rev Panam Salud Publica. 2011;30(5):490-500. Portuguese. https://doi.org/10.1590/s1020-49892011001100013
Fujishiro K, Ahonen EQ, Winkler M. Investigating Employment Quality for Population Health and Health Equity: A Perspective of Power. Int J Environ Res Public Health. 2022;19(16):9991. https://doi.org/10.3390/ijerph19169991
Arcoverde MAM, Berra TZ, Alves LS, Santos DTD, Belchior AS, Ramos ACV, et al. How do social-economic differences in urban areas affect tuberculosis mortality in a city in the tri-border region of Brazil, Paraguay and Argentina. BMC Public Health. 2018;18(1):795. https://doi.org/10.1186/s12889-018-5623-2
Walt G. Globalization and health. Med Confl Surviv. 2001;17(1):63-70. https://doi.org/10.1080/13623690108409556
Kamel AA, Ford PB, Kaczynski AT. Disparities in park availability, features, and characteristics by social determinants of health within a U.S.-Mexico border urban area. Prev Med. 2014;69 Suppl 1:S111-3. https://doi.org/10.1016/j.ypmed.2014.10.001
Quinn SC, Kumar S. Health inequalities and infectious disease epidemics: a challenge for global health security. Biosecur Bioterror. 2014;12(5):263-73. https://doi.org/10.1089/bsp.2014.0032
Gustafsson C. '"For a better life …" A study on migration and health in Nicaragua'. Glob Health Action. 2018;11(1):1428467. https://doi.org/10.1080/16549716.2018.1428467
Cerqueira MT. Health and human security in border regions. Rev Panam Salud Publica. 2012;31(5):362-4, 359-61. https://doi.org/10.1590/s1020-49892012000500002
Al-Soleiti M, Abu Adi M, Nashwan A, Rafla-Yuan E. Barriers and opportunities for refugee mental health services: clinician recommendations from Jordan. Glob Ment Health (Camb). 2021;8:e38. https://doi.org/10.1017/gmh.2021.36
Holst J, van de Pas R. The biomedical securitization of global health. Global Health. 2023;19(1):15. https://doi.org/10.1186/s12992-023-00915-y
Seo BR, Park SH. Policies to Promote Medical Tourism in Korea: A Narrative Review. Iran J Public Health. 2018;47(8):1077-1083. URL.
Sabo S, de Zapien J, Teufel-Shone N, Rosales C, Bergsma L, Taren D. Service learning: a vehicle for building health equity and eliminating health disparities. Am J Public Health. 2015;105 Suppl 1(Suppl 1):S38-43. https://doi.org/10.2105/AJPH.2014.302364
Rotker K, Velez D. Where will telemedicine go from here? Fertil Steril. 2020;114(6):1135-1139. https://doi.org/10.1016/j.fertnstert.2020.10.050
Manji K, Hanefeld J, Vearey J, Walls H, de Gruchy T. Using WhatsApp messenger for health systems research: a scoping review of available literature. Health Policy Plan. 2021;36(5):594-605. https://doi.org/10.1093/heapol/czab024
Su D, Wang D. Acculturation and cross-border utilization of health services. J Immigr Minor Health. 2012;14(4):563-9. https://doi.org/10.1007/s10903-011-9518-x
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Carlos Miguel Rios-González

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.