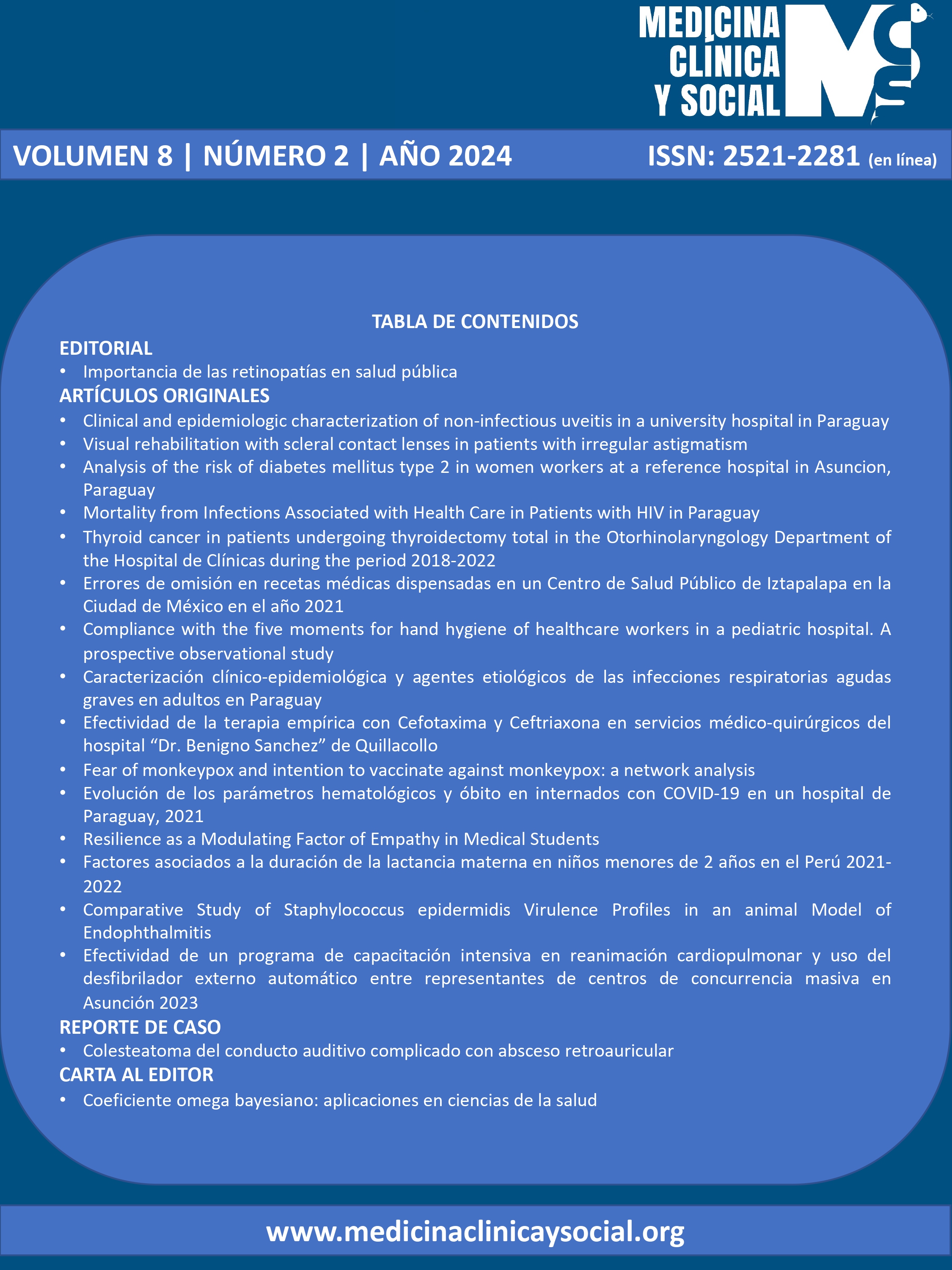
Compliance with the five moments for hand hygiene of healthcare workers in a pediatric hospital. A prospective observational study
DOI:
https://doi.org/10.52379/mcs.v8i2.367Keywords:
Hand hygiene, infection, prevention, health care workers, hospitalAbstract
Introduction: Healthcare-associated infections (HAIs), also known as nosocomial infections or hospital-acquired infections, begin within 48 hours of hospitalization, within 30 days after hospital discharge, or 90 days after undergoing surgical procedures. Objective: The study aimed to describe the compliance with the five moments for hand hygiene (HH) of the healthcare workers (HCWs) in a hospital. Methods: A prospective observational study was conducted from June 1 to 30,2020 in a pediatric hospital. HCWs compliance with the five moments of HH was registered by direct observation blindly to the participants, using the fact sheet for HH of the WHO. In the rows, the five moments of contact with the patients were recorded: before touching a patient, before clean aseptic procedure, after body fluid exposure risk, after touching a patient and after touching patient surroundings. The actions performed, also was registered: hand washing, alcohol hand friction, omission, or use of gloves. Data were analyzed in SPSS V 21. The protocol was approved by the institutional review board. Results: During the study period, 2.595 observations to 104 HCWs were made. They were pediatric residents 38.5 %, nurses 32.7 % and pediatricians 28.8 %. A global compliance with the five moments of HH of the participants were 64.5% (1673/2595). Before touching a patient, the adherence was 86,9%. The nurses adhered in 69%, pediatrician in 68.6 % and the pediatric residents in 57.2%. Discussion: The global percentage of compliance with the five moments of HH of the medical and nursing staff of the pediatric hospital was 64.5%. Nurses had the highest percentage of adherence. Handwashing compliance was higher before contact with the patients.
Downloads
References
Haque M, Sartelli M, Mckimm J, Bakar MA. Health care-associated infections – an overview. Infect Drug Resist. 2018;11:2321–33. https://doi.org/10.2147%2FIDR.S177247
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections: AMeta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039–46. https://doi.org/10.1001/jamainternmed.2013.9763
Liu JY, Dickter JK. Nosocomial Infections: A History of Hospital-Acquired Infections. Gastrointest Endosc Clin N Am [Internet]. 2020;30(4):637–52. https://doi.org/10.1016/j.giec.2020.06.001
Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, et al. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet. 2011;377(9761):228–41. http://dx.doi.org/10.1016/S0140-6736(10)61458-4
Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS One. 2017;12(12):1–18. https://doi.org/10.1371/journal.pone.0189621
Poudel AN, Zhu S, Cooper N, Little P, Tarrant C, Hickman M, et al. The economic burden of antibiotic resistance: A systematic review and meta-analysis. Vol. 18, PloS ONE 2023. e0285170 p. http://dx.doi.org/10.1371/journal.pone.0285170
Magill SS, O’Leary E, Janelle SJ, Thompson DL, Dumyati G, Nadle J, et al. Changes in Prevalence of Health Care–Associated Infections in U.S. Hospitals. N Engl J Med. 2018;379(18):1732–44. https://doi.org/10.1056/nejmoa1801550
Kim JS, Lee E. Difference between self-reported adherence to standard precautions and surveillance and factors influencing observed adherence: a quantile regression approach. BMC Nurs. 2022;21(1):1–9. https://doi.org/10.1186/s12912-022-00984-1
Lotfinejad N, Peters A, Tartari E, Fankhauser-Rodriguez C, Pires D, Pittet D. Hand hygiene in health care: 20 years of ongoing advances and perspectives. Lancet Infect Dis. 2021;21(8):e209–21. http://dx.doi.org/10.1016/S1473-3099(21)00383-2
Ng WK, Shaban RZ, van de Mortel T. Healthcare professionals’ hand hygiene knowledge and beliefs in the United Arab Emirates. J Infect Prev. 2017;18(3):134–42. https://doi.org/10.1177/1757177416677851
Irek EO, Aliyu AA, Dahiru T, Obadare TO, Aboderin AO. Healthcare-associated infections and compliance of hand hygiene among healthcare workers in a tertiary health facility, southwest Nigeria. J Infect Prev. 2019;20(6):289–96. https://doi.org/10.1177/1757177419848141
World Health Organization. WHO guidelines on Hand Hygiene in Health Care First Global Patient Safety Challenge Clean Care is Safer Care. URL
Sax H, Allegranzi B, Uc I, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007; 67:9-21. https://doi.org/10.1016/j.jhin.2007.06.004
Boora S, Singh P, Dhakal R, Victor D, Gunjiyal J, Lathwal A, et al. Impact of Hand Hygiene on Hospital-Acquired Infection Rate in Neuro Trauma ICU at a Level 1 Trauma Center in the National Capital Region of India. J Lab Physicians. 2021;13(02):148–50. https://doi.org/10.1055/s-0041-1730820
Herrera Travieso DM. Adherence to hand hygiene among helath workers. Rev Cubana Hig Epidemiol [Internet]. 2021;306(2021):57. URL
Maciel-Urzúa JA, Zamudio-Martínez G, Rangel-León G, Bustamante-Morales ME, León RADV De, Pérez-Navarro J V. Adherence to hand hygiene at five moments and specific protection in a tertiary care hospital during the COVID-19 pandemic.Gac Med Mex. 2021;157:313–7. https://doi.org/10.24875/gmm.m21000564
Krishnamoorthi S, Priyadarshi K, Rajshekar D. Impact of conducting hand hygiene audit in COVID-19 care locations of India—A large scalenational multicentric study – HHAC study. Indian J Med Microbiol. 2023;43:39-48. https://doi.org/10.1016/j.ijmmb.2022.09.002
De Arriba- Fernandez A, Molina- Cabrillana MJ, Serra.Majem L. Evalution of adherence to hand hygiene in health care professionals in a third level hospital in relation to the SARS-CoV-2 pandemic. Rev Esp Quimioter. 2021;34(3):214–9. https://doi.org/10.37201/req/150.2020
Rodríguez-Villar D, Del-Moral- Luque JA, Rodríguez-Caravaca G, Gil-de- Miguel A, Duran-Poveda M. Hand hygiene compliance with hidroalcoholic solutions in medical students. Cross-sectional study. Rev Esp Quimioter. 2019;32(3):232–7. URL
Musu M, Lai A, Mereu NM, Galletta M, Campagna M, Tidore M, et al. Assessing hand hygiene compliance among healthcare workers in six Intensive Care Units. J Prev Med Hyg. 2017;58(3):E231–7. URL
Lambe KA, Lydon S, Madden C, Vellinga A, Hehir A, Walsh M, et al. Hand Hygiene Compliance in the ICU: A Systematic Review.Crit Care Med. 2019;47: 1251–7. https://doi.org/10.1097/ccm.0000000000003868
Ojanperä H, Kanste I, Syrjala H. Hand-hygiene compliance by hospital staff and incidence of health- care-associated infections, Finland. Bull World Health Organ. 2020;98 :475–83. https://doi.org/10.2471/blt.19.247494
Landoas A, Cazzorla F, Gallouche M, Larrat S, Nemoz B, Giner C, et al. SARS ? CoV ? 2 nosocomial infection acquired in a French university hospital during the 1st wave of the Covid ? 19 pandemic, a prospective study. Antimicrob Resist Infect Control. 2021;1–8. https://doi.org/10.1186/s13756-021-00984-x
Asgill TF, Stupart D. Nosocomial bacterial infections in Victoria decreased during the COVID-19 pandemic.J Infect Prev. 2023;24(4):151–8. https://doi.org/10.1177/17571774231159383
Huang F, Armando M, Dufau S, Florea O, Brouqui P, Boudjema S. COVID-19 outbreak and healthcare worker behavioural change toward hand hygiene practices. J Hosp Infect. 2021;111(March 2020):27–34. https://doi.org/10.1016/j.jhin.2021.03.004
Ganesan V, Sundaramurthy R, Thiruvanamalai R, Raghavan M, Chavan SKD, Pusa R, et al. Hand Hygiene Auditing: Is It a Roadway to Improve Adherence to Hand Hygiene Among Hospital Personnel? Cureus. 2022;14 (5) e25221. https://doi.org/10.7759/cureus.25221
Hammerschmidt J. Nurses ’ knowledge , behaviour and compliance concerning hand hygiene in nursing homes?: a cross-sectional mixed- methods study. BMC Health Service Research. 2019; 19:547. https://doi.org/10.1186/s12913-019-4347-z
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Lorena Grau, Giselle Perruchino, Mirta Mesquita

This work is licensed under a Creative Commons Attribution 4.0 International License.