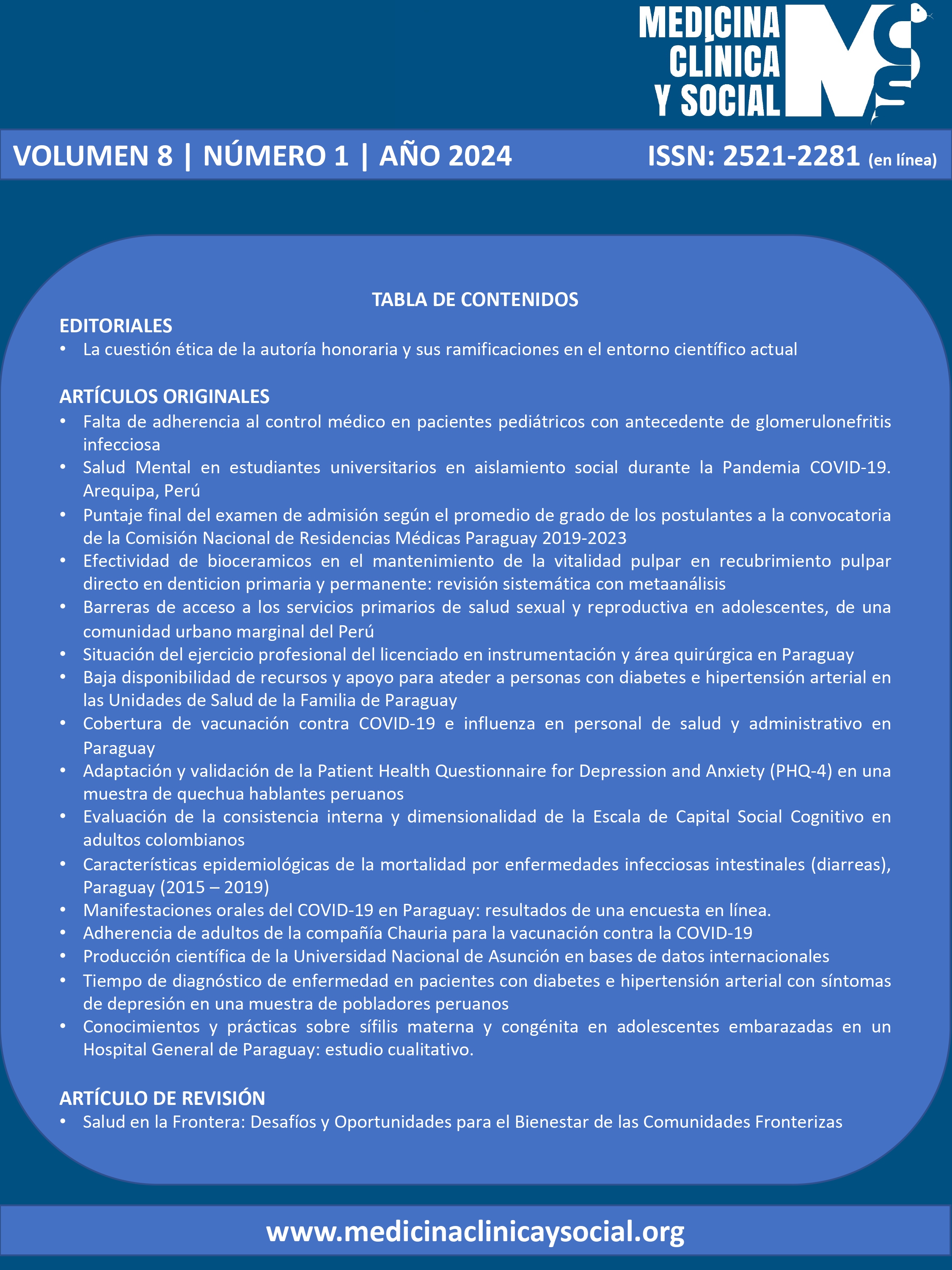
Oral Manifestations of COVID-19 in Paraguay: Results from an Online Survey.
DOI:
https://doi.org/10.52379/mcs.v8i1.370Keywords:
SARS-CoV-2, oral diagnosis, dysgeusia, xerostomia, mouth ulcersAbstract
Introduction: Previous studies have reported that patients infected with the COVID-19 virus could manifest symptoms in the oral cavity. Objective: To evaluate the frequency of oral manifestations associated with COVID-19 in a segment of the Paraguayan population and determine the most prevalent ones. Methods: Descriptive cross-sectional study. An electronic survey was conducted from January to March 2022. The data were presented as frequencies and percentages and analyzed using the chi-square test. Statistical analysis was performed with R software version 4.0.3. Results: The sample consisted of 478 individuals. 79.50% were female, and 45.19% were between 25 and 34 years old. 65.48% reported having experienced at least 1 oral symptom or sign during the course of COVID-19. The loss of the sensation of bitter tastes, followed by the alteration of the taste of foods and the loss of sweetness perception, were the most common symptoms. A significantly higher proportion of oral manifestations was found in the 18-24 age range (?²; p= 0.003). Among people who developed COVID-19 in a moderate to severe form, a greater number of oral symptom manifestations were observed (?²; p= 0.044). Discussion: A high frequency of oral manifestations was identified in patients with moderate to severe cases of COVID-19, with taste disorders standing out as the most predominant. Younger individuals were the most affected.
Downloads
References
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021; 19, 141–154. https://doi.org/https://doi.org/10.1038/s41579-020-00459-7
World Health Organization (WHO). Internet. Dashboard. Citado 1 de mayo de 2022. Disponible en: https://covid19.who.int
Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). En: StatPearls Internet. Treasure Island (FL): StatPearls Publishing; 2022. Citado 12 de mayo de 2022. Disponible en: http://www.ncbi.nlm.nih.gov/books/NBK554776/
Khamis AH, Jaber M, Azar A, AlQahtani F, Bishawi K, Shanably A. Clinical and laboratory findings of COVID-19: A systematic review and meta-analysis. J Formos Med Assoc. 2021;120(9):1706-18. https://doi.org/10.1016/j.jfma.2020.12.003
World Health Organization (WHO). Internet. Citado 8 de mayo de 2023. Disponible en: https://www.who.int/
Ejaz H, Alsrhani A, Zafar A, Javed H, Junaid K, Abdalla AE, et al. COVID-19 and comorbidities: Deleterious impact on infected patients. J Infect Public Health 2020;13(12):1833-9. https://doi.org/10.1016/j.jiph.2020.07.014
Zhang JJ, Dong X, Liu GH, Gao YD. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin Rev Allergy Immunol. 2023;64(1):90-107. https://doi.org/10.1007/s12016-022-08921-5
Zhu F, Zhong Y, Ji H, Ge R, Guo L, Song H, et al. ACE2 and TMPRSS2 in human saliva can adsorb to the oral mucosal epithelium. J Anat. 2022;240(2):398-409. https://doi.org/10.1111/joa.13560
Drozdzik A, Drozdzik M. Oral Pathology in COVID-19 and SARS-CoV-2 Infection—Molecular Aspects. Int J Mol Sci.2022;23(3):1431. https://doi.org/10.3390/ijms23031431
Gutierrez-Camacho JR, Avila-Carrasco L, Martinez-Vazquez MC, Garza-Veloz I, Zorrilla-Alfaro SM, Gutierrez-Camacho V, et al. Oral Lesions Associated with COVID-19 and the Participation of the Buccal Cavity as a Key Player for Establishment of Immunity against SARS-CoV-2. Int J Environ Res Public Health. 2022;19(18):11383. https://doi.org/10.3390/ijerph191811383
Sabbagh HJ, Abdelaziz W, Quritum M, Alamoudi RA, AlKhateeb NAB, Abourdan J, et al. A multi-country study on the impact of sex and age on oral features of COVID-19 infection in adolescents and young adults. BMC Oral Health. 2022;22:513. https://doi.org/10.1186/s12903-022-02515-5
Tuter G, Yerebakan M, Celik B, Kara G. Oral manifestations in SARS-CoV-2 infection. Med Oral Patol Oral Cir Bucal. 2022;27(4):e330. https://doi.org/10.4317/medoral.25259
Silveira FM, Mello ALR, da Silva Fonseca L, dos Santos Ferreira L, Kirschnick LB, Martins MD, et al. Morphological and tissue-based molecular characterization of oral lesions in patients with COVID-19: A living systematic review. Arch Oral Biol. 2022;136:105374. https://doi.org/10.1016/j.archoralbio.2022.105374
Martín Carreras-Presas C, Amaro Sánchez J, López-Sánchez AF, Jané-Salas E, Somacarrera Pérez ML. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. 2021;27(3):710-2. https://doi.org/10.1111/odi.13382
Sarasati A, Agustina D, Surboyo MDC. The Oral Lesion in the COVID-19 Patient: Is It True Oral Manifestation or Not? Infect Drug Resist. 2023;16:4357-85. https://doi.org/10.2147/IDR.S411615
El Kady DM, Gomaa EA, Abdella WS, Ashraf Hussien R, Abd ElAziz RH, Khater AGA. Oral manifestations of COVID-19 patients: An online survey of the Egyptian population. Clin Exp Dent Res. 2021; 7(5):852-860. https://doi.org/10.1002/cre2.429
Chawla J, Y N, Bakshi SS, Kalidoss VK, Yadav S, Polineni S, et al. Oral manifestations associated with COVID-19 disease: An observational cross sectional study. J Oral Biol Craniofacial Res. 2022;12(2):279-83. https://doi.org/10.1016/j.jobcr.2022.03.008
Nijakowski K, Wyzga S, Singh N, Podgórski F, Surdacka A. Oral Manifestations in SARS-CoV-2 Positive Patients: A Systematic Review. J Clin Med. 2022;11(8):2202. https://doi.org/10.3390/jcm11082202
Boscolo-Rizzo P, Polesel J, Vaira LA. Smell and taste dysfunction after covid-19. BMJ. 2022;378:o1653. https://doi.org/https://doi.org/10.1136/bmj.o1653
Mahmoud MM, Abuohashish HM, Khairy DA, Bugshan AS, Khan AM, Moothedath MM. Pathogenesis of dysgeusia in COVID-19 patients: a scoping review. Eur Rev Med Pharmacol Sci. 2021 Jan;25(2):1114-1134. https://doi.org/10.26355/eurrev_202101_24683
Ali FA, Jassim G, Khalaf Z, Yusuf M, Ali S, Husain N, et al. Transient Anosmia and Dysgeusia in COVID-19 Disease: A Cross Sectional Study. Int J Gen Med. 2023;16:2393-403. https://doi.org/https://doi.org/10.2147/IJGM.S408706
World Health Organization (WHO). Internet. WHO Coronavirus (COVID-19) Dashboard. Citado 26 de octubre de 2023. Disponible en: https://data.who.int/dashboards/covid19/cases?m49=600&n=c
Li H, Li Y, Liu J, Liu J, Han J, Yang L. Vaccination reduces viral load and accelerates viral clearance in SARS-CoV-2 Delta variant-infected patients. Ann Med. 2023;55(1):419-27. https://doi.org/10.1080/07853890.2023.2166681
Instituto Nacional de Estadística del Paraguay. Internet. 2023. Citado 26 de octubre de 2023. Disponible en: https://www.ine.gov.py/news/news-contenido.php?cod-news=1623
Brandini DA, Takamiya AS, Thakkar P, Schaller S, Rahat R, Naqvi AR. Covid-19 and oral diseases: Crosstalk, synergy or association? Rev Med Virol. 2021; 31(6):e2226. https://doi.org/10.1002/rmv.2226
Carrasco C, Vinitzky I, Román A, Vélez J, Morales V, Fernández R, et al. Disgeusia como principal manifestación oral en pacientes con COVID-19 leve en el Instituto Nacional de Enfermedades Respiratorias. Odontol Sanmarquina Impr. 2022; 25(1):e22064. https://doi.org/https://doi.org/10.15381/os.v25i1.22064
El Kady DM, Gomaa EA, Abdella WS, Ashraf Hussien R, Abd ElAziz RH, Khater AGA. Oral manifestations of COVID-19 patients: An online survey of the Egyptian population. Clin Exp Dent Res. 2021; 7(5):852-860. https://doi.org/10.1002/cre2.429
Binmadi NO, Aljohani S, Alsharif MT, Almazrooa SA, Sindi AM. Oral Manifestations of COVID-19: A Cross-Sectional Study of Their Prevalence and Association with Disease Severity. J Clin Med. 2022;11(15):4461. https://doi.org/10.3390/jcm11154461
Abubakr N, Salem ZA, Kamel AHM. Oral manifestations in mild-to-moderate cases of COVID-19 viral infection in the adult population. Dent Med Probl. 2021;58(1):7-15. https://doi.org/10.17219/dmp/130814
Reis VP, Bezerra AR, Maia ABP, Marques LC, Conde DC. An integrative review of oral manifestations in patients with COVID-19: signs directly related to SARS-CoV-2 infection or secondary findings? Int J Dermatol. 2021; 61(3): 278–290. https://doi.org/10.1111/ijd.15881
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Carlos Alberto Aguilera Núñez, Maria Gabriela Buccini Martínez, Nahomi Resedad Barreto Rodríguez, María del Carmen González Galván, Cynthia Mireya Jara Pintos

This work is licensed under a Creative Commons Attribution 4.0 International License.