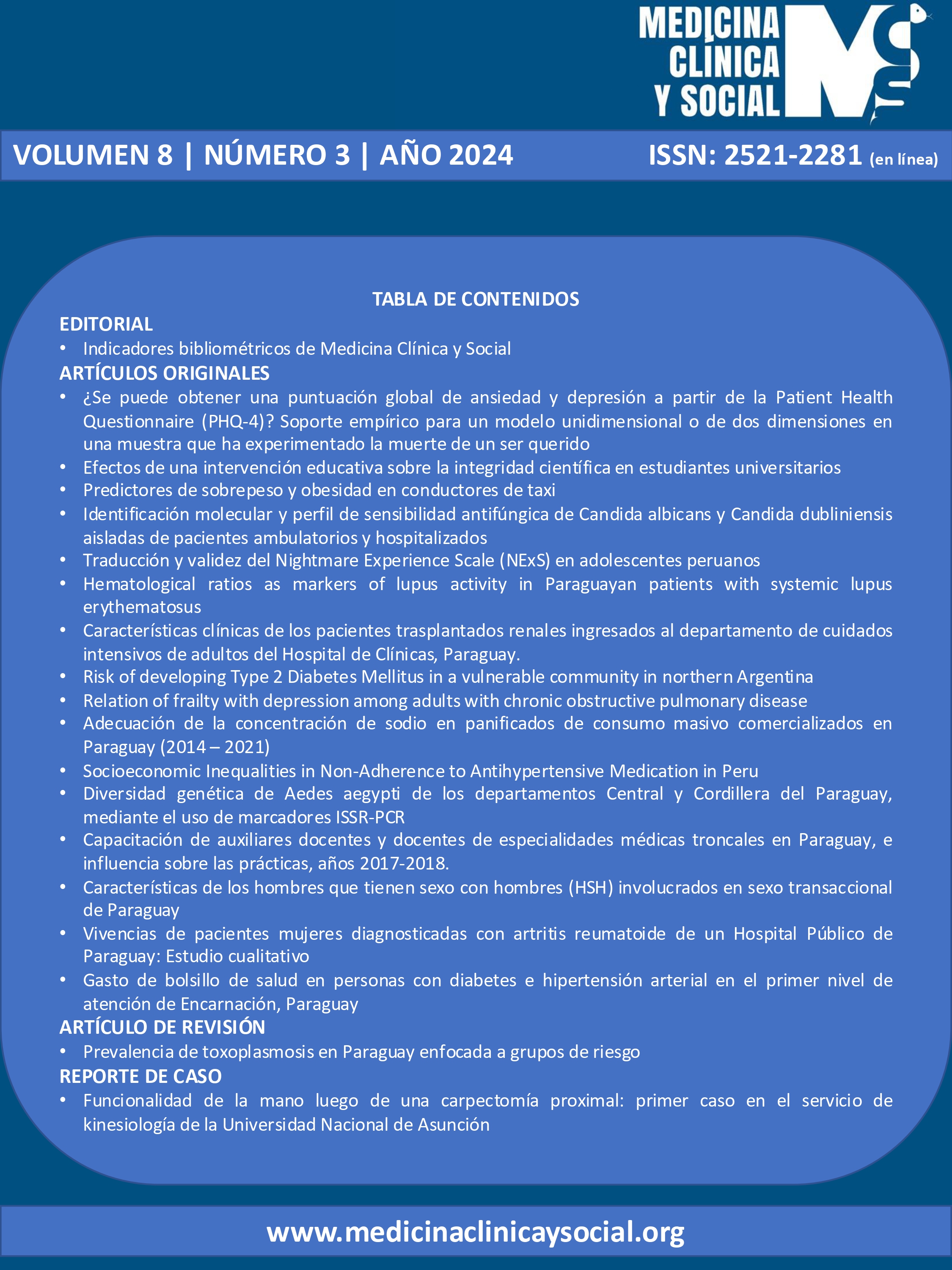
Risk of developing Type 2 Diabetes Mellitus in a vulnerable community in northern Argentina
DOI:
https://doi.org/10.52379/mcs.v8i3.447Keywords:
Diabetes mellitus, Type 2, Body Weight Changes, surveys and questionnairesAbstract
Introduction: Prevention of diabetes requires sustained lifestyle changes as well as identification of groups at higher risk. Objective: The aim of this research was to estimate the risk of diabetes in vulnerable subjects from a primary care center in northern Argentina, with no known glucose abnormalities, using the FINDRISC questionnaire, investigate the relationship between survey variables and the final score, and explore its association with metabolic risk factors and body composition. Methodology: This cross-sectional design included 498 patients without type 2 diabetes or known glycemic abnormalities. All subjects underwent a complete medical history and completed the FINDRISC questionnaire. Results: The predominant age group was 18-45 years old. Around 64% were physically active and 44% reported daily consumption of fruit and vegetables. Most of them had a BMI higher than 25 kg/m2. Regarding the risk of developing type 2 diabetes in the next 10 years, 24.3% were at low risk and the remaining fraction was distributed in slightly elevated, moderate, high and very high risk. All variables influenced the individuals' variance (p < 0.05). The hierarchical clustering and principal component analysis (PCA) revealed that elevated FINDRISC score was strongly associated with: age > 65 years, fasting blood glucose, BMI ? 30 kg/m2 and antihypertensives use. CONCLUTION: We found a high percentage of obesity and overweight, as well as a high risk of cardiometabolic disease and of developing T2D. In addition, in the population studied, the variables that compose the FINDRISC did not influence the highest score in the same way.
Downloads
References
Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, et al. Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci. 2020;21(17):6275. https://doi.org/10.3390/ijms21176275
Avilés-Santa ML, Monroig-Rivera A, Soto-Soto A, Lindberg NM. Current State of Diabetes Mellitus Prevalence, Awareness, Treatment, and Control in Latin America: Challenges and Innovative Solutions to Improve Health Outcomes Across the Continent. Curr Diab Rep. 2020;20(11):62. https://doi.org/10.1007/s11892-020-01341-9
Mendis S. Global status report on noncommunicable diseases 2014: World health organization. 2014. URL
Tang M, Chen Y, Krewski D. Gender-related differences in the association between socioeconomic status and self-reported diabetes. Int J Epidemiol. 2003;32(3):381-385. https://doi.org/10.1093/ije/dyg075
Hernández-Teixidó C, López-Simarro F, Arranz Martínez E, Escobar Lavado FJ, Miravet Jiménez S. Vulnerabilidad y determinantes sociales en diabetes [Vulnerability and social determinants in diabetes]. Semergen. 2023;49(8):102044. https://doi.org/10.1016/j.semerg.2023.102044
Carrillo-Larco RM, Aparcana-Granda DJ, Mejia JR, Bernabé-Ortiz A. FINDRISC in Latin America: a systematic review of diagnosis and prognosis models. BMJ Open Diabetes Res Care. 2020;8(1):e001169. https://doi.org/10.1136/bmjdrc-2019-001169
Obura MO, van Valkengoed IG, Rutters F, et al. Performance of Risk Assessment Models for Prevalent or Undiagnosed Type 2 Diabetes Mellitus in a Multi-Ethnic Population-The Helius Study. Glob Heart. 2021;16(1):13. https://doi.org/10.5334/gh.846
Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26(3):725–731. https://doi.org/10.2337/diacare.26.3.725
Vianna CA, da Silva Linhares R, Bielemann RM, Machado EC, González-Chica DA, Matijasevich AM, et al. Accuracy and adequacy of waist circumference cut-off points currently recommended in Brazilian adults. Public Health Nutr. 2014;17(4):861-9. https://doi.org/10.1017/s1368980013000529
Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1-17. https://doi.org/10.1007/978-3-319-48382-5_1
Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. 2019;62(1):3-16. https://doi.org/10.1007/s00125-018-4711-2
Gallardo-Rincón H, Cantoral A, Arrieta A, Espinal C, Magnus MH, Palacios C, et al. Review: Type 2 diabetes in Latin America and the Caribbean: Regional and country comparison on prevalence, trends, costs and expanded prevention. Prim Care Diabetes. 2021;15(2):352-359. https://doi.org/10.1016/j.pcd.2020.10.001
Magliano DJ, Boyko EJ; IDF Diabetes Atlas 10th edition scientific committee. IDF DIABETES ATLAS. 10th ed. Brussels: International Diabetes Federation; 2021. URL
Ministerio de Salud de Argentina [Internet]. Cuarta Encuesta Nacional de Factores de Riesgo Para Enfermedades No Transmisibles, 2018. http://www.msal.gob.ar/images/stories/bes/graficos/0000001622cnt-2019-10_4ta-encuesta-nacional-factores-riesgo.pdf
Brainard G. Is the Middle Class within Reach for Middle-Income Families? URL
Instituto Nacional de Estadística y Censos (INDEC). Informes técnicos. Vol 5, nº 59. ISSN 2545-6636. Condiciones de vida. Incidencia de la pobreza y la indigencia en 31 aglomerados urbanos. 2021. URL
Penfold M, Rodríguez Guzmán G. The Growing but Vulnerable Middle Class in Latin America. Growth Patterns, Values and Preferences. Public Policy and Productive Transformation Series. Caracas: CAF; 2014. URL
Tumas N, Rodríguez Junyent C, Aballay LR, Scruzzi GF, Pou SA. Nutrition transition profiles and obesity burden in Argentina. Public Health Nutr. 2019;22(12):2237-2247. https://doi.org/10.1017/s1368980019000429
Kojta I, Chaci?ska M, B?achnio-Zabielska A. Obesity, Bioactive Lipids, and Adipose Tissue Inflammation in Insulin Resistance. Nutrients. 2020;12(5):1305. Published 2020 May 3. https://doi.org/10.3390/nu12051305
Galante M, O´Donnell V, Gaudio M, Begué C, King A, Goldberg L. Epidemiological Condition of Obesity in Argentina. Rev Argent Cardiol. 2016;84(2):132-138. URL
Ruderman A, Pérez LO, Adhikari K, Navarro P, Ramallo V, Gallo C, et al. Obesity, genomic ancestry, and socioeconomic variables in Latin American mestizos. Am J Hum Biol. 2019;31(5):e23278. https://doi.org/10.1002/ajhb.23278
Ganz ML, Wintfeld N, Li Q, Alas V, Langer J, Hammer M. The association of body mass index with the risk of type 2 diabetes: a case-control study nested in an electronic health records system in the United States. Diabetol Metab Syndr. 2014;6(1):50. https://doi.org/10.1186/1758-5996-6-50
Atayoglu AT, Inanc N, Ba?misirli E, Çapar AG. Evaluation of the Finnish Diabetes Risk Score (FINDRISC) for diabetes screening in Kayseri, Turkey. Prim Care Diabetes. 2020;14(5):488-493. https://doi.org/10.1016/j.pcd.2020.01.002
Silvestre MP, Jiang Y, Volkova K, Chisholm H, Lee W, Poppitt SD. Evaluating FINDRISC as a screening tool for type 2 diabetes among overweight adults in the PREVIEW:NZ cohort. Prim Care Diabetes. 2017;11(6):561-569. https://doi.org/10.1016/j.pcd.2017.07.003
Ríos Rodríguez SJ, Gutiérrez Cueva R, Gutiérrez Ayala GIL, et al. Riesgo de desarrollar diabetes mellitus tipo 2 según escala Finnish Diabetes Risk Score en atención primaria. Rev Cubana Med Gen Integr. 2023;39(2). URL
Sosa ML, JaraCM, Pratt P, et al. Analysis of the risk of diabetes mellitus type 2 in women workers at a reference hospital in Asuncion, Paraguay. Med. clín. soc. 2024;8(2):141-147. https://doi.org/10.52379/mcs.v8i2.368
López-González ÁA, García-Agudo S, Tomás-Salvá M, Vicente-Herrero MT, Queimadelos-Carmona M, Campos-González I. Test FINDRISC: relación con parámetros y escalas de riesgo cardiovascular en población mediterránea española [FINDRISC Test: Relationship between cardiovascular risk parameters and scales in Spanish Mediterranean population]. Rev Med Inst Mex Seguro Soc. 2017;55(3):309-316. URL
Traoré S, Paré B, Dabourou D, Guira O, Sagna Y, Kamouni J, et al. Performance of the Finnish Diabetes Risk Score (FINDRISC) in the Identification of Dysglycemia in an Urban Population in Ouagadougou (Burkina Faso). Open J Int Med. 2021;11:39-54. https://doi.org/10.4236/ojim.2021.112003
Azzouz M, Boudiba A, Guerchani MK, Lyes Y, Hannachi R, Baghous H, et al. Apport du score de risque finlandais FINDRISC dans l’identification de la dysglycemie dans une population algeroise, Algerie. Médecine des maladies Métaboliques. 2014;8:532-538. https://doi.org/10.1016/S1957-2557(14)70877-6
Schmid R, Vollenweider P, Waeber G, Marques-Vidal P. Estimating the risk of developing type 2 diabetes: a comparison of several risk scores: the Cohorte Lausannoise study. Diabetes Care. 2011;34(8):1863-8. https://doi.org/10.2337/dc11-0206
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Mariano Nicolás Aleman, María Constanza Luciardi, Mariana Soledad Medina , Mariana Pera, Mirta Centeno Maxzud, Hector Lucas Luciardi

This work is licensed under a Creative Commons Attribution 4.0 International License.